1. Introduction
Preterm has been identified as a worldwide pandemic, with statistics showing that it is the second most frequent cause of death of infants under the age of five, globally: its survivors have also been seen to suffer lifelong ailments due to the shortened gestational length [97]. Preterm births also cause health complications to the mother alongside the foetus and have economic consequences which primarily stem from lifelong provision of care for its survivors, alongside clinical resources which are expended for care alongside false predictions [138,180]. Despite the global effects of the preterm pandemic, effective means of predicting the condition and understanding of its causes are lacking, the majority of which is due to the still growing knowledge and understanding of the uterine anatomy and its related physiology [60]. As preterm is viewed as a multi-factorial condition, its causes and associated effects (physiologically, economically and publicly) have been typically discussed, analysed and reviewed as individualistic components which makes it challenging for readers to be able to gain a rigorous and holistic understanding of the condition. In addition to this, from the published literature, a standard and accurate method towards the prediction of preterm appears to be lacking (I. B. [67]).
This manuscript is structured in two parts where a semisystematic methodology is adopted towards reviewing the topic of preterm births under multiple relevant discussion headings in the first part, from which a cybernetic framework towards preterm prediction and eventual control, and comprising a collaborative framework between and an AI model (prediction machine and care recommender) and a clinician is proposed, which is envisaged to provide prediction accuracies which supersede the current methods and allow for the delivery of optimised treatment to pregnant patients, which is believed to ultimately enhance the care strategies delivered. Specifically speaking, the contributions of this review study are as follows:
-
-
An extensive review of the concept of preterm under headings such as: what qualifies as a preterm birth, economic impacts, potential causes, ethnicity and preterm, genetics and preterm, current means of labour and preterm diagnosis, countries with high preterm, and survival rates.
-
-
A review of machine learning and AI in clinical practice is conducted and gives an overview on how these computational tools could lead to optimised care and treatment therapies.
-
-
This is followed by a proposition of a cybernetic framework which includes an AI model in the clinical loop to serve as a decision support tool and, in tandem with a clinical expert, forms a superintelligence framework for preterm prediction and associated care strategies.
-
-
The summary which drills down potential areas of future work which could be used to improve the overall performance of the cybernetic framework, which includes: the need for the further generation and consensual sharing of patient physiological data for further AI model building exercises to enable aspects to be improved, consideration of ethnicity in prediction models due to disparity in gestational lengths amongst various ethnicities, and the use of wearables for mobile and continuous monitoring of pregnancies using principles of telemedicine.
1.1. Human gestation, foetal membranes and physiology of uterine contractions
The onset of pregnancy commences when an egg successfully merges with a travelling sperm cell to yield a fertilised egg (also known as a zygote during the fertilisation process), after which, in a matter of days, the zygote travels to the uterus where its growth process commences [107,137,157]. During the growth process, the zygote initially goes through multiple cleavage divisions by first becoming a morula ball of cells before growing into a larger mass known as a blastocyst [107,137,157]. Around a week post fertilisation, the uterus discharges an enzyme that causes dissolution of the zona pellucida around the blastocyst, which thus leads the cell mass to attach to the uterine wall, resulting in an implantation [107,137,157]. Shortly after implantation the blastocyst invades the endometrium, leading to the trophoblast splitting into an outer syncytiotrophoblast and an inner cytotrophoblast [107,137,157]. The cells in the uterine stroma begin to multiply, giving rise to a cup like frame which grows across the blastocyst up until implantation is complete, and is termed the uterine decidua [107,137,157]. The syncytiotrophoblast encapsulates the growing embryo and serves as the main tissue which is in direct contact with the maternal tissue, and goes on to form the external layer of the placenta [107,137,157].
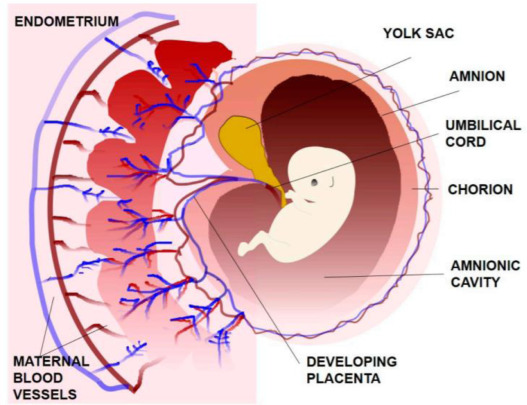
Three of the extraembryonic membranes, namely the yolk sac, amnion and allantois are produced within the inner cell mass [27,107]. The yolk sac is a lined membrane whose prime role is the supply of the embryo with blood cells, and surrounds the blastocoel, and the amnion is a single layered cell that grows over the developing embryo [27,107,137]. The amnionic cavity contains amniotic fluid whose prime role is to absorb mechanical shocks and waves propagated towards the direction of the foetus, while supplying nourishment [27,107,137]. The allantois is pouch like in nature and positioned at the end of the embryo, and ranges towards the umbilical cord [27,107,137].
In humans, the foetal membrane is the interface between the mother and developing foetus. The membrane provides protection of the foetus from mechanical shocks, agents and viruses during the pregnancy process, while also contributing towards hormonal regulation during the pregnancy phase [27,107,137,157].
During the onset of labour (term or preterm), a membrane activation takes place, thus a detachment of the amniotic membranes from the decidua which culminates in the rupture of the membrane [137]. An image showing a foetus within the uterus alongside the extraembryonic membranes can be seen in Fig. 1:
 Fig. 1
Fig. 1Viewing the pregnancy phase from a trimester point of view, the human pregnancy can be broken into three phases. During the first trimester, a host of changes begin to manifest themselves in the mother's body as a response to hosting a foetus, foetal development occurs leading to the onset of growth and development of the brain and genitalia and nerves as per the American College of Obstetricians and Gynaecologists (ACOG) (foetal Development, n.d.-a; foetal Development, n.d.-b; [159]). Due to the key, yet subtle, developments that take place to the foetus during the first trimester, this phase is said to be the timeframe where a large portion of birth defects and miscarriages tend to occur. The second trimester is characterised by foetal growth, and includes foetus expansion in the range of 3–5 inches, commencement of dynamic movements which can be felt by the mother, and the development of a sleep and circadian rhythm (foetal Development, n.d.-a; foetal Development, n.d.-b; [91] | Biology for Majors II, n.d.; [66,159]). Due to the developments which occur in the second trimester, this is the stage which the sex of the foetus can be determined with the use of ultrasound imaging (foetal Development, n.d.-a; foetal Development, n.d.-b; [91] | Biology for Majors II, n.d.; [66,159]).
In the third trimester (final phase prior to labour), the foetus can now be noted to respond to external stimuli from the environment (i.e. environmental light and sound) and the foetus appears to be more active within the womb, with more movements which can be felt by the mother (foetal Development, n.d.-a; foetal Development, n.d.-b; [91] | Biology for Majors II, n.d.; [66,159]).
A diagram showing the various foetal development stages across the three trimesters can be seen in Fig. 2:
 Fig. 2
Fig. 21.2. What is PT, effects of PT, epidemiology of PT
1.2.1. What is PT?
A preterm (PT) birth can be defined as one where the birth occurs before 37 completed weeks of gestation since the mother's last menstrual period, although the number ‘37′ is viewed as somewhat generic and arbitrary, as there are risks for babies who are born above the cut off number of 37 [89,119,121,126,217]. Preterm is viewed globally as a widespread cause of death, and loss of individual potential in certain cases amongst the survivors. Statistically speaking, preterm births account for around 35% of the deaths in children under the age of five, making it the second most common cause of death in children within that age range after pneumonia [89,119,121,126,217] Furthermore, babies born preterm have also been seen to carry a heightened risk of dying due to being more prone to neonatal infections [89,119,121,126], [217] This makes the case of preterm a Global Burden of Disease analysis due to the high mortality level and substantial risk of a lifelong impairment [89,119,121,126,217]. The long term consequences of preterm continue throughout the life of the survivors and the aftereffects include particular physical effects, neurodevelopmental impairments and family/socio economic effects as detailed in Table 1.
Table 1. Summary of the various effects of preterm birth.
| Outcome | Outcome category | Examples | References |
|---|---|---|---|
| Physical effects | - Visual handicap- Lung frailness- Long term cardiovascular vulnerability and communicable disease |
|
[23,100,123][177,188,208][53,117,232] |
| Behavioural and neurodevelopmental effects | - Executive function impairment- Delay of global development- Behavioural sequela |
|
[42,88,211][48,155,185][44,194] |
| Social and societal effects | - Knock on effect on family- Health service support- Intergenerational subsequence |
|
[31,71,104][19,145,198] |
Economic Implications of Preterm: as expected, the costs associated with managing preterm are largely dependent upon the extent of preterm. Statistics collected from the US suggest that an extreme prematurity costs in the scale of $100 K, $10–30 K for prematurity and under $4.5 K for a late premature birth [68,204]. For England and Wales, a joint statistic suggests the cumulative costs for society for the care of preterm births from delivery towards adulthood (18 years) are in the region of £3 billion, with the societal cost for a moderate preterm and extreme preterm being in the region of £62 K and £95 K [68,138]. The Italian National Health Service has estimated €58,098 as the cost to both the family and social security per preterm birth [35,68]. The bulk of the mentioned societal costs associated with a preterm birth stem from hospital costs and care costs, as can be expected. Other associated expenses which contribute toward the costs include follow on medication, costs due to specialist child care, and an increase in debt [68].
With the current means of preterm predictions being reported to be unstable and inaccurate, the accompanied cost from a false positive preterm that leads to hospitalisation costs approximately $20,000 per patient [68]. This is largely due to current preterm prediction methods being reliant on subjective means and data which largely causes false positives, leading to hospitalisation and provision of interventions which may not be required by the patient, so without doubt the improvement of effective prediction means results in economical and health based implications [68,132,133,131,167]. To phrase things in a more quantitative sense, van Baaren et al. conducted a model based study for the Netherlands where it was estimated that for a national delivery rate of 180,000 infants per year, a more stable and effective means of preterm prediction could lead to annual savings in the region of €2–€14 million per year [68,219].
1.2.2. Why/How PT occurs and causes
From a broad perspective, the concept of preterm can be sub-divided into two classes as follows: i) spontaneous preterm birth/premature rupture of membrane, and ii) initiated preterm birth, which implies birth through means such as a caesarean section or induction labour to cause birth to happen prior to the 37 week mark of gestation [20,76].
Spontaneous preterm births are a complex heterogeneous case which arise from a combination of genetic, physiological, environmental and lifestyle factors which give rise to transitions in the uterine state as it goes from quiescence to active contractions [75,149,154,175,209]. Being a heterogeneous process, it is challenging, if not near unfeasible, to pinpoint the sole factor behind the preterm birth in various pregnancy cases [75,149,154,175,209]. A number of subtle maternal factors which also contribute towards a preterm birth include low Body Mass Index, intervals between pregnancies and maternal age, and also include other lifestyle factors such as accumulated chronic stress, smoking and high alcohol consumption [75,149,154,175,209]. A contrasting table of the various types of preterm alongside some risk factors and associated interventions can be viewed in Table 2.
Table 2. Various types of preterm, risk factors, and interventions.
| Preterm type | Risk factors | Examples | Intervention examples | References |
|---|---|---|---|---|
| Spontaneous birth | - Age at time of conceiving- Multiple pregnancy- Disease and infections- Lifestyle |
|
Family planning in adolescence and preconception supportPolicy based rulings on certain aspects of artificial reproductive meansFrequent sexual health screenings and anti infection treatment plans for early mitigation of infections likely to occur during pregnancyCommunity based interventions for women of child bearing age, alongside antenatal care for proactive and early detections of complications | [43,90,174] |
| Provider initiated birth | - Caesarean section and medically induced labour for suspected foetal compromise, such as severe intrauterine growth restriction, twin to twin transfusion, and oligohydramnios. Maternal complications, i.e., pre-eclampsia, diabetes, epilepsy, and placenta previa |
|
Awareness campaigns have been put in practice in the hope of limiting the amounts of provider initiated births and caesarean sections | [152,153,205] |
A substantial distension of the uterus due to multiple pregnancies (i.e., twins, triplets etc.) has also been seen to be a risk factor of preterm, by a factor of 10 relative to a single birth [26,25,58,124,141,144]. Organically, multiple pregnancies have been seen to carry a 1 in 40 and 1 in 200 likelihood for West African and Japanese patients as an example, while artificial conception means have also been seen to cause multiple pregnancies in high income economies, leading to policy based constraints on the number of embryos that can be transferred during invitro fertilisation [26,25,58,124,141,144]. Unsurprisingly, infections are an active contributor towards an increased risk of preterm births, the list of which includes malaria, bacterial vaginosis, intrauterine inflammations, HIV and syphilis [26,25,58,124,141,144].
Provider initiated preterm is one the fundamental conditions related to preterm, although data and statistics for this are sparse and elusive, the clinical conditions underpinning medically induced preterm delivery include obesity, diabetes, renal disease, hypertension, uterine rupture, cholestasis, placental abruption, and preeclampsia [26,25,58,124,141,144].
1.3. Ethnicity in PT
Studies have shown that obstetric outcomes vary depending on the ethnic group of the patients, with notably more patients of Black ethnicity having a shorter gestation length by about five days, with the maternal ethnicity being the key factor as supposed to the father's [16,82,166,168,171,200,214]. A common notion as to why this is the case typically sees inferences from ethnic history and socioeconomic risk factors – studies have investigated this more closely and the results appeared consistent despite an adjustment for socioeconomic risk factors, with Africans having the highest rate of caesarean sections [16,82,166,168,171,200,214]. Interestingly, gross motor skills development occurs at an accelerated pace in black infants in comparison to Caucasian infants, which is likely due to a compensational effect due to having a shorter gestation span [98].
Patel et al. [168] conducted an ethnicity based preterm study with a broad sample size consisting of about 122,000 women of which 80% were Caucasian Europeans, 13% were Asian and 6% were Black. The Asian group comprised of nationals from India, Pakistan and Bangladesh, and the Black group comprised of Black Africans and Black Caribbean nationals (R. R. [168]).
The Carstairs index, which is a widely used indicator of material deprivation, showed that a higher level deprivation existed amongst the Black and Asian Groups when benchmarked against the Caucasian group. Smoking was seen to be more prevalent in the Caucasian group, while Black women reportedly had a higher than average Body Mass Index (BMI) and statistically were more likely to be obese.
The results also echoed previous knowledge with, in a general sense, Black ethnicity being the most prone to preterm delivery, followed by Asian and Caucasian ethnicities (R. R. [168]; Public Health Scotland, n.d.). Although the public health data on when preterm happens is sparse and difficult to come by, work done by R. R. [168] provides insightful statistics into this.The results in Table 3 provide a greater insight and granularity into ethnicity based statistics around maternal age and preterm births. Table 3 shows the various age at which there exists a heightened proneness to a preterm birth amongst the various ethnicities, from which it can be seen that Black women have a greater proneness to preterm when they deliver under the age of 20, Asian women are more prone to deliver preterm in the age range of 20–29, while for Caucasian women they are more prone in the over 30 age range.
Table 3. Percentage of preterm deliveries chunked by maternal age range and ethnicity (R. R. [168]).
| Maternal age range | Caucasian% preterm delivery | Black% preterm delivery | Asian% preterm delivery |
|---|---|---|---|
| Under 20 | 14 | 17 | 12 |
| 20–29 | 56 | 61 | 68 |
| Over 30 | 29 | 21 | 18 |
Taking into account the higher than average BMI in Black women, it was seen that even when BMI was in the normal range, Black women were still 33% more prone to deliver preterm when benchmarked against Caucasian Europeans, thereby suggesting a genetic predisposition for preterm births in Black women (R. R. [168,179]). For Asians with an increased likelihood of preterm, the key drivers of their preterm births include smoking and lack of support when compared to Caucasians, thus implying that physiological and psychological factors account for some of the causes of preterm in Asian women (R. R. [168]).
Acknowledging the subtle differences in the pregnancy timeframes in various ethnicities could have potential to inform clinical and precision based care to pregnant patients. Apparent instances where this could be applicable include the administering of steroidal injections in later stages of gestation, based on the average gestation period. In this case, ethnicity informed precision care would indicate that, due to Black infants maturing earlier, this course of treatment may not be directly relevant and would likely not compromise foetal survival (R. R. [168]).
Taking into account the varied gestation periods amongst ethnicities, a redefinition of what entails a ‘term’ birth could also be necessary as this influences whether follow up care is administered to a patient, and also if they are placed in the ‘high risk’ group with a likelihood of a subsequent pregnancy complication (R. R. [168]). The results and data have made apparent that an appreciation for subjective gestational timespans amongst different ethnicities could be useful towards achieving customised, necessitated and precision based obstetric care amongst pregnant patients (R. R. [168]).
Pelvic anatomy is a factor that has been indirectly linked to the gestational disparities between ethnic groups, where preliminary results by Betti [17] and Betti and Manica [18] show variations between birth canal and geometry of the pelvis from individuals from different regions, and due to the proximity of the uterine to the pelvis, this is presumed to have an influence in gestational lengths and births as a whole.
1.4. Genetics in PT
As a means towards explaining the variations in gestation lengths due to ethnic differences, research has been done on a genetic scale contrasting gene differences between Black and Caucasian ethnicities [6,72,75,143,142,206]. Allele and holotype frequencies have been potentially identified as gene frequencies which have influence on birth, but immediate research has implied that these gene frequencies do not independently cause preterm birth [6,72,75,143,142,206].
Due to the complexity of preterm births, it can be viewed as a polygenic condition, thereby suggesting that it is unfeasible for a single genetic marker to be the sole driver behind the condition – due to this, genetic factors are studied alongside a secondary factor [62,77,113,134,203,213]. The gene environment is a category which is often looked at and explores genetic disposition due to external environmental factors. With an infection induced preterm delivery, the primary genes responsible for immune modulation could provide a platform towards classifying ethnic subtleties in infections and preterm delivery [45,51,63,105,201].
Differences in gene frequencies responsible for physiological regulation have been hypothesised as a potential contributor to ethnic disparities in preterm [10,41,50,79,112,165,190]. Factors such as placental blood flow, foetal growth rate and preeclampsia condition, and ethnic differences are thought to play a role in vascular functionalities, and stress responses which are likely to contribute towards preterm births and foetal growth rate [10,41,50,79,112,165,190]. Individuals who belong to Black ethnicity have been shown to have a greater resting blood pressure and a heightened vascular response to external stress when compared to Caucasians–the vascular reactivity pathway poses an avenue which stress and associated responses could contribute towards preterm delivery [10,41,50,79,112,165,190].
In essence it can be inferred that genes which play a role in inflammations and vascular interventions indirectly play a role in preterm delivery as well. Despite this, it remains an active challenge to succinctly identify whether these genes are the sole contributors to the variations in gestational timespans between ethnicities, as genetic polymorphs alongside their frequencies between ethnicities would also need to be taken into consideration [37,129,151,187,201]. Polymorphisms study would need to identify polymorphs which vary in broad ethnic samples, and are independently associated with singular ethnicities – all samples would also need to be normalised against genetic confounding [37,129,151,187,201].
To summarise, there are signs that genes indirectly influence preterm delivery to an extent, but it remains challenging to attribute genetic factors to be the primary cause behind the ethnic difference in gestation length [62]. Polymorphism frequencies, which are responsible for immune regulations, have been noted to substantially vary between ethnicities, although it remains that a preterm delivery is a complex and heterogeneous process which is dependent upon a number of maternal genes, foetal genes and environmental subtleties [36,62,129,172]. Thus, due caution needs to be taken in order to not incorrectly suggest that genes are the key drivers behind the variational gestational length in ethnic minority, as this could produce the false belief that the condition cannot be remedied [62].
1.5. Methods of diagnosing gestation age and labour/How it is measured
The capability of being able to assess and quantify gestational age is important to evaluate obstetric outcomes and also ties in with perinatal epidemiology [4]. Ultrasound imaging is deemed to be the more reliable of the available means used in gestational age assessment [2,135,216]. With the assumption that conception takes place on the same day as ovulation, a retrospective technique which calculates the gestational age from the last menstrual period is also used, but has been critiqued for having a low accuracy, due to variability in the conception timeframe, and of course an uncertainty margin in the estimation of the last menstrual period [116]. Other alternatives to the last menstrual period estimate of gestation also include birthweight and fundal height [20].
An ensemble method which applies ultrasound imaging alongside an estimate of the last menstrual period, and known as ‘best obstetric estimate’, has also been used in assessing gestational age – as it is an ensemble method its accuracy supersedes that of either of the individual methods involved in the procedure [25,164]. A summary table containing the various recognised assessment methods can be seen in Table 4.
Table 4. Summary of various recognised gestation age assessment methods.
| Assessment | Uncertainty range | Principle | Disadvantage | References |
|---|---|---|---|---|
| Early trimester ultrasound | +/- 5 days when done within first trimester+/- 7 days when done after first trimester | Scans are typically done within weeks 6–18 of pregnancy and involve a qualitative observation of foetal biometric factors such as crown-rump length, biparietal diameter etc. | - High instrument cost for ultrasound alongside a trained expert- Ultrasound accuracy is limited if foetus is malformed or mother's Body Mass Index is above a score of 35 | [13,108] |
| Obstetric estimate | +/- 10 days | Algorithmic estimate using inputs deduced from an ultrasound scan and the last menstrual period | - Lack of a standardised computation algorithm amongst various organisations | [25,164] |
| Fundal height | +/- 21 days | Distance from symphysis to fundus is measured | - Accuracy is similar to last menstrual period method | [12,13,108,158,186] |
| Estimation of last menstrual period | +/- 14 days | Mother estimates last menstrual period | - Largely ineffective in low resource areas with low literacy- Largely influenced by variation in ovulation | [191,210,215] |
| Birthweight inference of gestational length | Best estimate is for babies born < 1500 g | Weighing of baby upon birth | Confusing for ethnicities whom are predisposed to weigh lighter at birth i.e. certain Asian ethnicities | [64,202] |
| Assessment of new-born | +/- 13 days dependent on index score utilised | Typically involves neurological assessment of the baby alongside indices such as Parkin, Fallan and Dubowitz | Subjective method highly reliant on level of competency and expertise of assessor | [20] |
- Reactive diagnosis of preterm: the concept of reactive preterm diagnosis is based on the identification of a preterm condition using active and prevalent markers and symptoms in the pregnant patient. The typical diagnosis of preterm is based on the standard devised by the American College of Gynaecology, and looks at symptoms such as uterine contraction regularity, cervical dilation and effacement [3]. Uterine contraction pattern is classed as preterm if ≥ 4 within 20 min or ≥ 8 within 60 min, if cervical dilation is greater than 3 cm, or if transvaginal ultrasound is used and the cervical length is in the range of 20–30 mm [128,132].
The methods for diagnosing preterm are largely viewed as erroneous and unreliable due to how they are performed alongside the notion that a number of the preterm diagnosis symptoms can also be present in nonpreterm pregnancy patients (I. B. [67]). It is said that in certain regions, only about 10% of pregnant patients diagnosed with conventional preterm means actually deliver within a week of the diagnosis (I. B. [67]).
The following is a summary of the leading methods in the diagnosis of preterm:
-
-
Cervical length: cervical length has statistically been shown to be a reasonable predictor for preterm with a shortened cervix closely being correlated with shorter pregnancies, with ultrasound imaging being the recognised acceptable means of length measurement [14,15,87]. A general rule of thumb is that the risk of preterm is inversely proportional to the length of the cervix, where a shorter cervix length insinuates a greater risk factor [14,15,87].
-
-
Biochemical markers: fluidic emissions which range from urine, amniotic fluid, cervical mucus and saliva, to name a few, are some of the biological emissions which have been used in the prediction of preterm, while in some scenarios, a combination of acquired fluid and cervical length have been used as a means of prediction of preterm [30,54,84]; K. [124,147]. Tests are also done for the analysis of glycoprotein in the vaginal secretion around the third trimester in a test called the foetal fibronectin test, its effectiveness in determining due date for a suspected preterm birth has been seen to be in the range of 7–10 days (foetal Fibronectin Test - Mayo Clinic, n.d.; [86]). However, there are studies which have expressed scepticism about the use of fluidic emissions to predict preterm, as the consensus states that no combination of biochemical markers would be able to sufficiently and reliably predict preterm delivery [176].
-
-
Contraction frequency: the occurrence of frequent uterine contractions has been viewed as a feature which can be used to predict a preterm delivery. This method has been seen to carry appeal as it allows for a mobile health monitoring platform which could allow for effective monitoring while reducing on the number of hospital visits made by the pregnant patient [94,92,93]. From a broad perspective, the challenge associated with this approach is intertwined with the contraction instrumentation used, candidates of which include Electrohysterogram and Tocogram, both of which have their own unique strengths and limitations [68,192].
A number of other methods exist for the prediction of preterm but there still continues to be no standardised or unanimously accepted method of predicting preterm birth [30,160,170].
1.6. Where it happens
Worldwide estimates of preterm by the World Health Organisation have stated that in 2010, 135 million live births occurred worldwide, with over 11% preterm, a considerable amount – 60% of which occurred in sub-Saharan Africa and Asia [20,22]. In addition to an apparent disposition for a shorter gestation span, this has also been attributed to higher fertility and a greater number of births in these areas relative to the rest of the world [20]. From an income centred perspective, in descending order, preterm have been seen to be prevalent in low income countries, low middle income countries, upper middle and finally high income countries [20]. The top ranked countries from a preterm birth perspective include India, China, Nigeria, Pakistan, Indonesia, United States, Bangladesh, Philippines, Democratic Republic of Congo and Brazil [21,20]. The cumulative sum of preterm births from these 10 countries account for 60% of all the preterm births worldwide [20]. As can be expected, survival is seen to be highest amongst the babies born preterm who had prompt accessibility to quality medical care. To put things into perspective, a study around the year 1990 showed that in a high income country where babies were born after only 28 weeks of gestation, 66% of these babies survived with a minimal accompanying long term impairment [120,150,189]. At the other extreme, in low income countries only 30% of babies born after 28–32 weeks survived, where a reported majority born after less than 28 weeks of gestation went on to die within their first few days of birth, with new born deaths accounting for a substantial proportion of deaths in low income countries [20,120,150,189], thus echoing the need for improved medical care globally.
The above statistics make it apparent that even though preterm is indeed a global pandemic, there exists a considerable survival gap for babies depending on the economic status of the regions in which they are born [20,120,150,189]. It has also been seen that a combination of an upsurge in socioeconomic elements alongside antenatal care contributed towards the decrease of preterm births in the 1960s–1980s in high-income countries such as France, Scotland and Finland [20,120,150,189].
It is typically seen that babies born at less than 28 weeks require an intensive neonatal care scheme at the minimum to enable them to survive, while the babies born within 28–32 weeks require specialist care [24,115]. The quality of these kinds of care in low and some middle income countries continues to be poor and has formed part of the causes which have given rise to the survival gap [24,115].
In addition to the crucial immediate impact of being able to save the lives of babies, further incentives to tackle the issue of preterm birth across all gestational lengths, a greater awareness of the long term implication of the surviving babies, their family wellbeing and associated cost of care for the disabled individuals throughout their lifetime within the society needs to be taken account [21,89,125,173,229,231].
1.6.1. Part 1 summary
In Part 1, various aspects surrounding the [91] and preterm births have been reviewed. Pregnancy commences when a fusion of the egg occurs with a sperm in transit to yield a zygote, which after forming finds its way towards the uterus where the growth process begins. The pregnancy and gestation process is split into three phases, where each phase is characterised by unique growth characteristics in the foetus.
Preterm birth has been defined here as a scenario where birth occurs prior to 37 complete weeks of gestation. It is recognised as a global pandemic and is the second most prominent cause of death in children under the age of five. For cases where the child survives preterm birth, lifelong physical and neurological impairments usually follow, in addition to psychological distress on the family.
Economic and financial implications have been seen to follow preterm from a care perspective, this has been summarised in Section 1.2.1. in Part 1, where mock simulation studies have shown that cost saving benefits in the region of €2–14 million per year are to be gained with an effective and proactive preterm prediction framework.
Ethnicity and genetic factors behind preterm were reviewed, where it is seen that ethnic minorities, i.e., Black and Asian ethnicities have an apparent tendency and predisposition to deliver earlier than mothers of Caucasian ethnicities, thereby implying that ethnic considerations need to be taken into account in order for customised and precision based care to be administered to different patients in the face of a potential preterm birth. Ethnicity informed strategies for risk grouping of patients would also allow for a more efficient grouping of patients into risk groups, with likelihood for a subsequent pregnancy complication.
A review of potential genetic markers which contribute to birth disparities between ethnicities finds that no single genetic marker is pivotal enough to give rise to the variable gestational lengths between ethnicities, due to the multifactorial complexity of the process. Even though genetic differences exist in physiological regulations in different ethnicities that implicitly contribute towards foetal growth and gestation, care needs to be taken to not conclusively suggest that genetic differences are the cause of shorter gestational lengths and therein preterm delivery, as this would lead to the false impression that preterm is a condition that cannot be actively remedied.
A number of the frequently used means of predicting preterm birth, primarily involving the estimation of the length of the cervix as a means of predicting risk of preterm, have been reviewed and, along with analysis of various fluids for biochemical markers and, more recently, the analysis of contraction patterns using instrumentations such as Electrohysterogram and Tocogram.
Global statistics conducted by the WHO showed that 11% of the global births in the world are preterm where subSaharan Africa, the USA and Asia account for 60% of this. Survival of preterm babies has been seen to be low in low income countries in comparison to high income countries who have more quality healthcare facilities, which strongly improves the odds of survival of new born preterm babies. This implies that, in addition to preterm being a global pandemic, there exists a survival gap of preterm babies in low and high income countries, which in turn is dependent on the economic capability of a country to provide a high standard of care to its patients.
1.6.2. Part 2–Potential Cybernetic solution
As a first step towards more effective care strategies for preterm births and foetuses, it is apparent that more effective birth prediction strategies are required [176]. As no single biomarker or sole qualitative phenomenon can be used as a reliable means of predicting preterm, a substantial amount of attention is now being shown to the contraction signals from the uterine muscle during the onset of labour of birth [60,61,70,69,97,109,178]. In its most fundamental form, the uterus is an anatomical tissue made up of cells forming part of a wall whose key roles include supporting the bladder, alongside ejection from the womb during labour [60,61,70,69,97,109,178].
Around the onset of the third trimester, uterine contractions have been seen to commence, the magnitude and frequency of which intensify all the way towards labour and culminates in birth [85,184]. The dynamics of the contraction of the uterine muscles involve cellular depolarisation and an instantaneous generation of a bioelectric signal typically in the mV scale, and is regarded as an action potential [85,184].
As preterm prediction is often viewed as a multifactorial prediction problem, it has been said that the dynamics of the uterine contraction signals are a function of the various physiological factors which contribute in an unknown weighted fashion towards the prediction of preterm birth, thereby making it arguably the richest source of information that can be used in determining a likely preterm birth [85,184]. Even though there continues to exist a gap in the understanding of the link between the biophysics of uterine contractions and the associated bioelectric manifestation, signal acquisition instrumentation alongside nonlinear signal processing methods have made it possible to infer and estimate the state and condition of a foetus from an acquired uterine contraction signal [60,61,70,69,97,109,178]. The realisation of the promise offered by uterine contraction signals through the effective acquisition and analysis of the acquired signal has led to databases hosting various kinds of physiological signals acquired from term and preterm patients during the third trimester of pregnancy [52,59,74,101].
Published results from the work done using the dataset from these sources have produced positive results and promising potential applications, but the shortcomings of the published case studies have continued to show that the preterm prediction problem is treated in isolation as a binary based classification problem (term/preterm) [9,56,55,60,61,70,69,97,109,178,232]. The contributions have continued to be prediction artificial intelligence (AI) models as opposed to a system whose framework can be deployed in a clinical setting and in collaboration with clinicians to proactively regulate preterm and enhance care strategies for the identified pregnant patients at risk with the designed AI model playing an integral role [9,56,55,60,61,70,69,97,109,178,232].
With this in mind, in this section we apply the principles of cybernetics to show how a design prediction machine (AI model) can work in collaboration with clinicians to foster a form of superintelligence framework augmenting AI with human intelligence (clinicians) in a loop for a more informed and proactive decision making platform which can potentially minimise preterm births, allow for safer deliveries and serve as an informative tool for potential resource and care allocation in the face of the birth of an extreme preterm foetus [161,227].
This framework of intelligence would be implemented using a trained prediction machine model from acquired uterine signals that will work in tandem with a therapy recommender system pending a predicted preterm, both of which can be viewed as the AI component of the loop. The output and recommendation of the AI model is passed on to the clinical expert who can assess the information and potentially pick up on likely false positives, or modify the AI proposed therapy based on expert knowledge prior to treatment, thereby serving as the human expert/human intelligence within the prediction and therapy recommendation decision flow [130,161]
. A qualitative sum of the respective contribution of the AI model and the human expert will ultimately yield a superintelligence platform whose prediction and treatment recommendation stem from an augmented intelligent source whose decision supersedes that of its individual counterpart, and would allow for appropriate and personalised care strategies to be delivered in a timely fashion. All of the above mentioned serve as sub components for a cybernetic loop which facilitates the end to end regulation for optimal outcome of the process in question [28,33,118,136,196,197,199]. Details of this are articulated further in the subsequent section, and a diagram showing the various subcomponents within the cybernetic framework can be seen in Fig. 3.
 Fig. 3
Fig. 31.7. Need for AI models in modern medicine
Within medicine as a whole, there exists a number of areas which operate inefficiently. Examples of this include: lack of efficient resource allocations, administering of wrong treatment and misdiagnosis, all of which has led to a rise in the need for AI models within the clinical workflow [47,78,96,106,122,169,225,228]. AI could provide support in the allocation of resources in clinical settings based on patient needs, and serve as a means of decision support by combining both qualitative and quantitative information prior to reaching a diagnosis, the applications of which span obstetrics, cancer, and mental health to name a few, thereby potentially minimising error rates in clinical practices when the appropriate AI model is utilised [47,78,96,106,122,169,225,228]. This is achieved by a computational process known as learning; in addition to this the AI mechanism is self-capable of further learning from failed attempts using additional user initiated processes [95].
AI models can be primarily implemented using machine learning (ML) and natural language processing (NLP) models [46,106,156]. For the application discussed in this paper, ML models are the frequently used approach and are the subject of further discussions [106]. ML models can be split into supervised and unsupervised approaches. Supervised learning thus far appears to be the favoured approach in clinical practice and involves the provision of labels to data samples prior to training; examples of these kinds of models include regression models, artificial neural networks, support vector machines and discriminant analysis to name a few [103,111,114]. While unsupervised learning allows for a self learning process from the perceived trend in the data without any prior expert labelling, examples of these methods include Gaussian mixture models and k-means clustering [103,162].
Data classification exercises span various ML models which include regressions, SVM, k-nearest neighbour, discriminant analysis, and to a lesser extent artificial neural network [103]. It can also be noted that advanced variants of the artificial neural networks (i.e. deep learning) have only sparsely been applied in the area of obstetric medicine when compared with areas such as ophthalmology and dermatology, as in this area of medicine model decision explainability is a requirement for the Food and Drug Administration (FDA) if these models are going to be eventually deployed in a clinical setting – thus, as artificial neural networks are black box based classifiers, these modes are only sparsely used in this area [57]. These criteria by the FDA have thus made it apparent to emphasise on areas such as the signal processing of the physiological signals, i.e., signal deconvolution methods and feature extraction for effective modelling, and effective tuning of nonblack box classifiers, for an efficient design of predictive models.
Similar to the CC-Cruiser AI prototype model by Long et al. [130], the proposed cybernetic framework (discussed in the subsequent section) where the AI model makes a prediction followed by a treatment and care recommendation which goes to the clinician to validate or take further action where necessary. Any inaccurate predictions made by the AI model, which in turn are detected by the clinician, would prompt further feedback action to the AI model to help improve and enhance its prediction accuracy [130]. Recent of examples of approved AI models for clinical applications include the following; CT brain bleed diagnosis tool (Aidoc), paramedic stroke diagnosis tool (Neural Analytics), atrial fibrillation detection (Apple), and MRI brain interpretation (Icometrix) [7,34,99,102,130].
1.8. Cybernetics and control
The word cybernetics stems from the Greek word kybernetes, and refers to the concept of systematically guiding the behaviour and state of a system towards an engineered outcome. Mathematician Norbert Wiener formalised this concept in his 1948 book titled ‘Cybernetic, or Control and Communication in the animal and the machine’ [83,227]. Although originally devoted to overlay the interaction between subcomponents in a system, as well as characterise functional autonomy in engineered machinery systems, modern day cybernetics has now evolved into a framework in which the interactions between nonlinear and complex processes (biological, organisational and societal) can be projected and analysed [8,224]. Key innovators towards the establishment of cybernetics include Margaret Mead, W. Ross Ashby, John von Neumann and Claude Shannon [8,181].
It has been seen that hierarchies exist within a cybernetic framework, with each level giving rise to a level of synthesis depth and thus a unique perspective on the subcomponent interactions within the system. Principally speaking, two orders are said to exist within cybernetics, namely the first and second order [65,73,83,223].
In first order cybernetics the key emphasis is on the mechanisms and element of feedback which is used to drive the ‘states’ of the system in question towards a desirable outcome given uncertainties and external disturbances [65,148]. This level of cybernetics is closely associated with technical tools including control theory, which emanates from the seminal work done by James Clerk Maxwell [146], and involves the steering of a system state using feedback controllers, which are models or agents that operate in tandem with a state estimation platform on the system with the principle of the minimisation of a detected error information signal, as assessed from the system and indicative of a deviation of the system trajectory from the desired pathway. From an abstract perspective, it can be said that the effectiveness of the control strategy implemented by the controller hinges upon the quality of the estimate of the states produced by the state estimation platform, which receives measurement signals from the system to produce its estimates. Thus, the state estimation represents a key component of the feedback element and control strategy [40,39].
Common methods used to estimate the state of a system include state observers, statistical time series state estimation methods and intelligent systems approaches which hinge upon machine learning and AI methods [5,32,195]. The intelligent system approach has been adopted for the cybernetic framework for the preterm monitoring and control method discussed as part of this paper, and will be discussed further in a subsequent section.
Second order cybernetics involves a more macro scale perspective of the analysis of the systemic interaction under the influence of feedback regulation. Second order cybernetics does not delve into the depths of the feedback process itself but acknowledges this as part of the whole system [65,83]. As second order cybernetics is focused around a system under the influence of a cybernetic framework, it can also be viewed as a meta cybernetic process and thus is also referred to as the ‘Cybernetics of Cybernetics’ [65,83].
Both orders of cybernetics are used as an analysis tool to critique the proposed system regulatory framework proposed for preterm prediction with a view to control. In the first order cybernetic view, we introduce the controller, which performs a mitigatory action to the system based on the estimated state to keep the system within a desired trajectory and desired outcome. The system in this case is a patient with a predicted preterm and the controller is a midwife (working within the multidisciplinary team of obstetricians and neonatologists) who administers the relevant care and therapy interventions (Nsugbe, Obajemu, et al., Unpublished results). In a subsequent section, the role and importance of feedback within the loop is described, as well as the interaction between the AI interface, which makes the birth prediction, and the human expert (obstetrician) who verifies and further customises the output from the AI machine (to form a superintelligence platform) prior to passing on to the midwife (controller) (Nsugbe, Obajemu, et al., Unpublished results).
Building on this, a macro scale overview will be given of the end to end operation of the proposed framework, making sense of the overall flow within the loop, and likely limitations. This will serve as the analysis of the proposed second order cybernetic methodology framework.
1.8.1. First order cybernetic analysis
This section details and analyses the proposed cybernetic operating framework as proposed by Nsugbe, Obajemu et al. (Unpublished results) for preterm monitoring, and shows the interaction between subcomponents within the loop such as midwife, pregnant patient, prediction machine (AI) and clinician, along with their various functions and interactions, with the core aim of predicting preterm alongside enhancing care strategies offered to patients. A view of the first order cybernetic framework under the influence of a superintelligence feedback mechanism can be seen in Fig. 4.
 Fig. 4
Fig. 41.8.2. Subcomponents of the cybernetic feedback loop
- Pregnant Patient (system): the system in a loop presents the central core which the remaining subcomponents are structured around, optimising and regulating. In this case study, the pregnant patient at any point in the third trimester (26+ weeks) represents the system. The third trimester has been chosen as this is the point in the pregnancy where uterine contractions of a considerable magnitude begin to propagate from the source towards the surface, and can be recorded using appropriate physiological instrumentation. The desired outcome in terms of ‘performance’ of the system is for the birth of a term foetus or a healthy foetus where a preterm birth occurs (Nsugbe, Obajemu, et al., Unpublished results). This will be achieved using a combination of a preterm prediction mechanism alongside a customised base care, as will be discussed subsequently. Sources of external perturbation, interferences and disturbances to the system which may reduce the potency and effectiveness of the care given to the pregnant patient include factors which influence the physiology of the pregnant patient, and thus the foetus, such as diet and lifestyle to name a few.
- Physiology Measurement: under the proposed framework, this point represents the stage at which physiological signals from uterine contractions are acquired from the pregnant patient. These signals in turn are used to determine whether a preterm delivery is predicted to take place. The acquisition of physiological signals typically involves the placement of electrodes on the surface of the myometrium while data is being collected: although not exhaustive, it has been seen in the literature that three key physiological instrumentations have been used, and are described as follows. Where required, the acquired physiological measurements from this stage can be combined with other medical based instrumentation such as cardiotocography and ultrasound sensors.
A summary of these can be seen in Table 5.
-
1)
Electrohysterogram (EHG): this instrumentation acquires the bioelectric signals resulting from cellular depolarisation from uterine contractions. These contractions, on average, commence during the start of the third trimester and intensify all the way towards labour, which culminates in the birth of a foetus. On a cellular scale, the governing principle of the dynamics of bioelectrical signal propagation is the Hodgkin-Huxley cellular electrophysiological model [85,184]. The major shortcomings of EHG as a means of contraction signal acquisition is the attenuation of the bioelectric signal as it travels from the source to the surface of the myometrium, due to tissue conductivities [163,221,222]. An image of an EHG recording from a pregnant patient can be seen in Fig. 5.
 Fig. 5
Fig. 5 -
2)
Tocogram (Toco): this instrumentation measures the mechanical offset, which is seen to follow the contraction of the uterus, and the propagation of bioelectric signals. The instrumentation contains a spring loaded pressure sensor which is used to record the mechanical displacements, and is typically placed on the fundus of the uterus during signal acquisition (Nsugbe, Obajemu, et al., Unpublished results; [193,220]). The Toco has been used more frequently as an auxiliary information source to support EHG recordings and allow for a fusion of information sources for prediction robustness, i.e. bioelectrical and biomechanical (Nsugbe, Obajemu, et al., Unpublished results; [193,220]). The shortcoming of this instrumentation is that the Toco effectively measures secondary manifestation of bioelectricity from uterine contractions, which could be assumed to limit the richness of the resulting signal.
-
3)
Magnetomyogram (MMG): the phenomena of electromagnetism extends itself towards bioelectrical signals, which allows for an accompanying magnetic field to follow the flow of ionic current within the tissue, which comes from action potentials associated with the contraction of the uterine muscles. In contrast to the more frequently used EHG, the propagation of MMG signals is not dependent upon anatomical tissue conductivities [9,56,55,232]. An image of an EHG recording from a pregnant patient can be seen in Fig. 6.
 Fig. 6
Fig. 6
Table 5. Summary of the three main instrumentations used in the measurement of physiological signals of uterine contractions.
| Instrumentation | Operating Principle | Advantage | Disadvantage | References |
|---|---|---|---|---|
| EHG | - Acquisition of bioelectric signal due to cellular depolarisation during anatomical contractions | - Low cost and simple to use | - Bioelectric signals are prone to attenuation due to tissue conductivities | [85,163,184,221,222] |
| Toco | - Mechanical signals from uterine contractions | - Low cost- Relies on mechanical displacements of uterine anatomy | - Effectively measures the secondary manifestations of a bioelectric source signal | (Nsugbe, Obajemu, et al., Unpublished results; [193,220]) |
| MMG | - Magnetic offset signals resulting from flow of ionic current within tissue | - Robust to signal attenuation from tissue conductivities | - Requires a large number of electrodes (100+)- Expensive- Prone to interferences from external magnetic sources | [9,56,55,232] |
As seen in the cybernetic loop diagram in Fig. 4, the data acquired at this stage feeds into the subsequent stage where predictions are made on the delivery state of the patient. Thus, care needs to be taken to ensure that high quality physiological recordings from the uterine muscle are acquired during this stage. Potential sources of error and uncertainties which may be superimposed on the signal during acquisition include motion artefacts and quantisation errors (De Anza, n.d.). However, it can be said that the effect of these sources of uncertainties are almost negligible in comparison to the overall quality of the signal.
Prediction Machine and Therapy Recommender: this is the point where the AI portion of the loop plays its role. This section can be split into two portions, one which describes the configuration and action of the prediction machine, and the other which articulates the constrained optimisation function and property employed by a proposed therapy recommender.
The prediction machine is expected to work with a machine learning (ML) algorithm where, given a set of acquired physiological signals from the candidate instrumentations mentioned in the prior section, a signal processing and classification exercise will need to be carried out to classify and differentiate the signals into classes of term or preterm, primarily based on the acquired signals (alongside qualitative information from patient medical health records). The acquired physiological signals typically take the form of a stochastic time series signal whose feature extraction warrants the need for statistical norms, predictive, frequency, entropy and fractal based features [80].
The prediction machine is the explicit part of the proposed cybernetic system which has been through an experimental validation of sorts, notably involving either EHG or MMG uterine contraction signal sources, Nsugbe et al. have produced a number of studies around the design of various kinds of prediction machines with generally high prediction capability and also have a degree of model interpretability and therein a reasonable likelihood towards obtaining FDA approval [161].
Following a pregnancy state prediction by the prediction machine, where a likely preterm has been identified, an optimiser runs through an optimisation exercise to suggest a recommended course of care and therapy for the pregnant patient. As proposed by Nsugbe Obajemu et al. (Unpublished results), the framework for the optimiser can be in the form of a constrained optimisation exercise where patient specific (i.e., ethnicity) and financial factors would be taken into account in order for the model to provide a recommendation which is relevant and customised towards the needs of the patients, as part of strides towards delivering precision based care for pregnant patients. For this problem, a mixture of metaheuristic and evolutionary based algorithms can be employed as a solver for the constrained optimisation problem [1,226]. Eq. (1) shows a sample mathematical optimisation formulation that contains a sample number of variables:
Where x is a value for a recommended drug and accompanying dosage, y is a value representing a therapy care measure, while z is an ad hoc measure which can be taken to provide further support where necessary for the patient, is a regularisation/penalty term, in this case is a care function encompassing various care based options(as defined by x,y,z) that need to be solved in order to yield the most optimum care strategy and approach given a set of defined constraints, represents a financial constraint, and is a patient specific physiological constraint, where the constraints are applied to reduce the algorithmic search space and ensure that the recommended output is one which is feasible both financially and physiologically (UWO, n.d.). Note that further constraints could be included as part of the optimisation problem depending on the clinical organisation and immediate factors.
As the output from the AI model feeds directly into a human interface, care needs to be taken to ensure that the output is comprehensible by the human expert professional. The key role of the AI model within this cybernetic loop includes the prediction of preterm by a quantitative model-based prediction from physiological data (and patient health record where applicable), followed by a recommended course of care and treatment given financial and patient physiological constraints.
Clinical Expert Validation: this sub block represents both the stage where the clinical expert takes action and the human intelligence aspect of the feedback mechanism within the cybernetic framework. The role of a clinical expert here can be likened to that of an optimal state tracker within a control theoretic sense, whose role is to smooth out estimates and predictions from theoretical knowledge of a system's behaviour [127]. The clinical expert, most likely an obstetrician, is expected in this case to use expert knowledge to closely analyse and look to validate the prediction and recommendation made by the AI system. The benefits of having the clinical expert in the loop serves to ensure that human intervention is part of the decision making process, which is essential for this part of clinical practice, adds a protective layer of ethical viability to the process to promote the best outcome while also serves to identify and remedy false predictions made by the AI model.
From a broad sense, the clinician at this stage has three prime actions that can be taken: 1) the acceptance of the prediction and recommendation made by the AI model; 2) the rejection of any predictions and recommendations identified as a likely false positive/negative; and 3) further consultation with the patient where a definite decision cannot be reached. Note that where predictions made by the AI have been deemed as false, this information would need to be utilised as further learning for the AI model in order to improve its overall efficiency.
Controller: this stage signifies the point where an action is applied to the system based on the estimated deviation from the desired outcome [110]. The controller in this case is assumed to be a clinical midwife whose role is to implement what is recommended by the combination of the AI model and clinician, both of which superimpose to yield a superintelligence platform, as mentioned. By the time the care recommendation gets to the midwife, it can be assumed that the patient physiology would have altered slightly due to time lapse from when the uterine data was acquired which was used to formulate the care recommendation by the AI model and clinician. This time lapse could span days to weeks, depending on the turnaround time. Because of this, the midwife can be said to possess the autonomy to modify slightly the course of care and treatment administered with respect to the amount of time elapsed between the acquisition of the uterine signals and the administering of the care and treatment in accordance with their professional regulations [207].
1.8.3. Effect of time delays on the cybernetic framework
From a control theoretic sense, time delays refer to the difference in time between the perception of a system's state and the accompanying execution of a responsive action on the system [49,182]. From an intuitive and practical perspective, time delays are generally unwanted within the loop as their effects could lead to redundant controller actions due to time lags [49,182].
As in the case with digital control systems, time delays in the context of the proposed framework can contribute towards the reduction of the anticipated effectiveness of the care which is provided by the midwife. The annotations in Fig. 4 show the areas within the loop that are likely to be influenced by time delays, the sum of which can be expressed as follows:
is the total amount of delays within the loop, and represents a source of delay within the loop.
From Fig. 4, the three sources of time delays within the loop can be defined as follows:
-
-
= assuming an offline post processing platform, this first delay arises from the delay between the acquisition of the uterine contraction signals and the eventual post processing. An estimated range of time delay that would be accrued at this stage will vary between 1 and 2 days.
-
-
= assuming there is no detected false prediction, it is anticipated that this process could take in the range of 1–2 days, depending on the availability of the expert clinician within the clinical setting. Note that at this stage the expert clinician may also seek an additional expert opinion here if needed, but it is anticipated that an upper cumulative time requirement in days should not exceed 2.
-
-
= this final delay within the loop arises from the interval between the midwife receiving the recommended course of treatment for the patient, and the patient attending a scheduled appointment. Although it can be assumed that patients with a detected imminency would have a quicker turnaround time for an appointment, it can be said that potential time delays at this point could span the range of 1–4 days.
Summing up all sources of delays mentioned, it can be said that an estimated 3–7 days would have lapsed to produce a time delay which would undoubtedly influence the effectiveness of the treatment provided to the pregnant patient. These time delays would undoubtedly manifest themselves in the form of further physiological variations from that which was initially recorded, alongside minor changes in the foetus. It can also be noted that in the case of a detected preterm with an associated close imminency timeline, the delays are expected to be significantly shorter as there would be prioritisations made to get the patient in the clinical setting to provide the prompt and relevant care.
Therefore, in order to ensure maximum effectiveness and appropriate care for the patient, the final care action to be administered by the midwife can be mathematically expressed as the following sum:
Where is the final care action to be delivered by the midwife, is the recommended treatment and course of therapy action, is a term used to account for time delays, and is an uncertainty term to account for any unforeseen issues encountered on the day of administering treatment, which also needs be considered.
In the UK/Ireland, if there is a threatened or potential preterm labour the delays would most probably be significantly shorter. Pregnant patients who present with a likely third trimester onset of labour are routinely administered steroid therapy to mature foetal lungs and magnesium sulphate for neuroprotection. The patient is required to remain as an inpatient for these therapies as they require additional monitoring. Obstetric input or neonatal team input would be ongoing. Due to the financial cost involved in providing appropriate care to preterm neonates, the team would be liaising with the midwifery staff regularly throughout the patient's stay in hospital. If necessary, there would also be input from other maternity teams if there was a chance that the host hospital was unable to provide a cot space for the neonate in the event of a preterm birth. Due to lack of bedspaces, pregnant patients can be transferred intranatally between hospitals.
1.8.4. Second order cybernetic analysis
Due to uncertainties, time delays and physiological factors, it can be acknowledged that it is unlikely that the proposed framework would be adept enough to completely eradicate the effects of preterm on mother and foetus. Rather, a more feasible and realistic objective for this proposed framework includes proactive care, with the overarching aim of greatly minimising the risk and complications which have a likelihood of occurring given a preterm circumstance. From the perspective of control theory, the goal is to drive the states of the system towards a more desirable outcome, which in this case translates to the following:
-
-
Proactive detection of preterm with less diagnosis subjectivity
-
-
Provision of care interventions to mother and foetus to delay extreme preterm birth where possible, alongside the provision of prompt care interventions to ensure foetus survival and safe delivery by the mother
From the macro based perspective of the second order cybernetic system flow, the ‘end to end’ operation of the framework can be succinctly described as the noninvasive acquisition of physiological signals from uterine contractions which account for the ‘observed phenomena’, and which is then processed through an AI model that provides a recommended course of care and treatment intervention given a predicted preterm scenario. This, in turn, is fed to a human expert within the process who assesses, critiques and modifies where necessary, in addition to being on the lookout for likely false predictions etc. With an anticipated outcome in mind, the final validated prediction and course of treatment is in turn passed to the midwife, who also goes on to modify the treatment course as required, and apply the care intervention agreed with the multidisciplinary team in accordance with current protocols.
As the pregnancy state prediction and recommended therapy is a function of AI and human intelligence, as mentioned, this superimposes together to yield a superintelligence based prediction and care recommendation platform. As a means of benchmarking the effectiveness of the overall proposed cybernetic framework, the following criteria can be used:
-
-
Number of false predictions leading to false hospitalisation
-
-
Prediction effectiveness across ethnicities
-
-
Preterm foetal and maternal survival rate
-
-
Ad hoc associated clinical birth drivers
1.9. Summary, and what can be accomplished
As no single qualitative approach or biomarker has been proven to be effective enough in the prediction of preterm, uterine contraction signals obtained during the third trimester of pregnancy have been shown to be compound signals which carry information that can be decoded with effective signal processing methods and used as a means of no subjective prediction of preterm birth. Although the biophysical knowledge of the uterine system continues to be a growing area, data driven approaches which rely on signal processing and machine learning are capable of mapping the relationship between an input stream of data and a respective pregnancy state prediction, thereby forming an AI model based prediction system.
This AI model is proposed to be one which is capable of making preterm predictions alongside recommending a course of care and therapy for the patient using a constrained optimisation structure. It has been proposed that this AI model sits with a clinical framework flow which comprises a human expert. The inclusion of AI models in clinical medicine can provide strides towards the eradication of subjectivity, misdiagnosis, and promote efficient means of resource allocation. A framework for how the AI model can be included in a clinical setting and be part of a cyber/human collaboration where AI and human intelligence are collaborated to yield a superintelligence was proposed with multiorder cybernetics (systematic guidance and steering towards a desired outcome).
Applying the principles of cybernetics, the first order implementation produced a loop as shown in Fig. 4, the framework comprises a system: a pregnant patient in third trimester, a measurement platform which acquires physiological signals from uterine contractions, an AI model comprising of a ML system used for preterm prediction alongside an optimisation driven recommendation system, a clinical expert who embodies the human intelligence which is part of the final decision making process in the feedback portion of the loop, and finally the controller – a midwife who is the front end party who applies the required treatment and care to the pregnant patient. The midwife is expected to take into account unforeseen uncertainties alongside time delays when offering care and treatment, and refer concerns to the wider team to ensure the implementation of appropriate action in a timely manner.
The second order cybernetics provide a philosophical framework from which the objectives and end to end operation of the proposed framework can be analysed, and its performance measured. A summary of the objective of the proposed framework is the reduction of subjectivity in diagnosis, with the inclusion of the AI model alongside the provision of prompt and personalised care to the pregnant patient. The key drivers, which can be used to access the overall effectiveness of the proposed framework have been fleshed out.
It is thought that with the proposed cybernetic framework for preterm monitoring, the following primary factors are achieved:
-
-
A general reduction of preterm within a set region alongside personalised and effective care
-
-
Personalised, effective and proactive care strategies
-
-
Economic and cost saving benefits due to the reduction of false predictions and unrequired care actions
-
-
Proactive care to new born foetuses which could reduce health complications encountered later in life, alongside reduced financial burden to the economy as a whole
-
-
Reduced physiological ‘knock on’ effects to mothers who deliver preterm due to active care strategies