1. Introduction
The aim of tissue engineering is to assemble constructs that provide mechanical, cellular, and molecular signals in order to restore, maintain, or improve damaged tissues or whole organs. Therefore, bone tissue engineering strives to restore a normal physiology or to speed up healing of bone in musculoskeletal disorders, injuries or deformities. Nowadays, autografts and allografts are commonly used in clinics in restorative therapy. However, bone harvesting is traumatic, causes pain and infections at the donor site, and very often results in complications. Hence, the use of synthetic grafts is emerging as an alternative treatment. Potentially, candidate materials for bone substitutesare a bioresorbable or biodegradable polymers and among them polyurethanes (PUR). PURs are non-toxic, biocompatible, biodegradable and they calcify in vivo. Properties of the PURs can be shaped by the various chemical compositions in the wide range of mechanical properties from rigid to flexible. Very broad assortment of products like foams, coatings, fibers, films etc. can be obtained from them [1], [2]. PURs support cell adhesion and proliferation of human osteoblasts and other cell types [3]. PURs are very important biomaterials in tissue engineering. Numerous publications describing the possibility of PUR application in bone regeneration are published each year. There is a need to give critical review over current status on this subject. Thus, the aim of this work is to present why PURs are one of the most prominent materials in the bone tissue engineering application. Different PUR systems will be discussed in terms of biodegradation, calcification, biological activity taking into account their various applications in bone repair.
2. Bone structure and repair
Bone is a specific form of connective tissue, composed of collagen scaffold impregnated with calcium salts Ca2 + and PO43 − [4]. Bones protect the internal organs, act as a lever to which muscles are attached. Bone tissue is constantly resorbed and replaced with a new tissue. This process removes small defects and allows the bone to remodel in response to pressure and gravity loads. In the adult, healthy human about 10% of bone is replaced within a year, which implies that approx. after 10 years bone composition is exchanged at 100% [5]. Bone is also an important reservoir of calcium, 99% of this element present in our body is localized in this tissue.
2.1. Bone structure
The bone consists of cells (approx. 5% by weight of tissue), and extracellular matrix (ECM) (Fig. 1). Osteoblasts or osteogenic cells (20–30 μm) differentiate from bone marrow stem cells. They produce organic components of ECM: collagen and proteoglycans, and secrete proteins that regulate bone mineralization process [4]. Osteocytes are an osteoblasts surrounded by an impermeable, mineralized bone matrix, and their main role is to exchange nutrients and metabolites in the bone, but also they act as mechanosensors. Through numerous canaliculi, osteocytes remain in contact with each other and with cells on the bone surface (Fig. 1b). Osteoclasts or osteoclastic cells (up to 100 μm) are multinucleated and of hematopoietic origin. Their main function is bone resorption which is controlled by enzymes - hydrolases, that decompose the organic bone components by acidification of the surrounding environment with H+ and Cl− ions [4].

Fig. 1. Schematic bone structure.
Reproduced with permission from The American Association for the Advancement of Science [6].Bone ECM is made up of organic component - approx. 30%, and inorganic component of 70% of dry weight. Organic components include primarly collagen type I, but also proteoglycans and other matrix proteins such as growth factors (GFs), which regulates bone mineralization. The hydroxyapatite (HA) is the major component of inorganic phase (60–70% of bone mass) and is localized in the ECM in the form of small crystals (10 × 15 nm) (Fig. 1d).
The first type of bone formed developmentally is woven bone (immature), later replaced by lamellar bone (mature) and is further classified as two types: trabecular bone (also called cancellous or spongy bone) and compact bone (also called dense or cortical bone). The cancellous bone is located at the ends of the long bones as well as at the core of vertebral bones in the spine, the pelvic bones, ribs, and skull. It is built from bone trabecules, which size and shape depend on the direction of force acting on the bone and contains bone marrow. The cortical bone is located in the external layer of flat bones and in the diaphysis [4]. Selected physical properties of cancellous and cortical bone are presented in Table 1.
Table 1. Selected physical properties of cancellous and cortical bone [7], [8].
| Property | Bone type - direction | |||
|---|---|---|---|---|
| Cortical - longitudinal | Cortical - transverse | Cancellous - longitudinal | Cancellous - transverse | |
| Porosity [%] | 5–10 | 75–90 | ||
| Density [g/cm3] | 1,99 | 0,05–1,0 | ||
| Volume fraction [mm3/mm3] | 0,85–0,95 | 0,05–0,60 | ||
| Young Modulus [GPa] | 17–20 | 6–13 | 20 | 14,7 |
| Tensile strength [MPa] | 79–151 | 51–56 | 10–20 | |
| Compression strength [MPa] | 131–224 | 106–133 | 2–12 | |
The outer surface of the bones (with the exception of the articular surface) is covered with a periosteum, while the inner surface, from the medullary canal side with a endosteum. The periosteum is built from connective tissue, which contains collagen fibers and a large number of cells, including stem cells, which are capable of dividing and can differentiate into osteoblasts. There are nerves and blood vessels as well, therefore periosteum also provides nourishment. Endosteum forms a film separating the trabecules from the medullary cavity. It contains both mesenchymal and hematopoietic stem cells, and together with periosteum residing cells takes part in bone remodeling and repair of bone defects.
2.2. Bone repair
In depth understanding of injured bone healing process lays at the base of biomaterials design for bone regenerative purposes. Bone healing consists of three consecutive processes: inflammation, repair and remodeling phases. To ensure bone regeneration, interplay between four elements need to be provided: 1) osteoconductive matrix (tissue scaffold); 2) osteoinductive signals (growth factors), 3) osteogenic cells (osteoblasts and stem cells); and 4) supply of blood and nutrients [9].
Osteoconductive, osteoinductive and osteogenic properties posses autologous bone graft. Autologous bone grafts have excellent biologic and mechanical properties, however their application may cause donor site morbidity, chronic postoperative pain, nerve damage and the limited volume available. The goal of tissue engineering is to assemble constructs that provide mechanical, cellular, and molecular signals in order to restore, maintain, or improve damaged tissues or whole organs. Scaffolds play a very important role in tissue engineering, by providing appropriate support for tissue growth and cell proliferation [10]. In 2010 Kommareddy et al. have proposed a mechanism of bone tissue regeneration on scaffolds [11]. The first stage is dominated by cell adherence and is highly dependent on the scaffold surface properties, such as chemistry and topography [12], [13]. Next, cells proliferate and migrate into the pores. After a delay time of a few weeks, which depends mainly on material stiffness, cells begin to form an ECM. Seeding density has a dramatic effect on the delay time, because cells need time to proliferate before they can migrate into the pores. When the cell seeding density is increased, cells take a very short time to reach confluence and the migration starts much earlier resulting in little dependence of the delay time on pore parameter. The extracellular tissue layer is thick enough to support the cells independent of the scaffold and the growth kinetics depends only on the interaction between the cells and their own ECM, not the scaffold material properties.
To summarize, during bone regeneration both structure and properties of the material and cell-material interactions are critical. There are already published some reviews describing bone tissue scaffolds requirements, in example those written by Carvalho et al. describing the interactions between cells, scaffolds and signaling molecules, and providing extensive information on bioactive constructs requirements [14], by Puppi et al. about design, synthesis, characterization of polymeric scaffolds for bone repair [15], by Pilia et al. giving comprehensive review on commonly used ceramics and polymers in bone repair [16], and by Janik and Marzec discussing benefits and drawbacks of classical scaffold fabrication methods [1]. Firstly, the physiochemical and mechanical properties such as appropriate biodegradability or bioresorbablity and mechanical properties adjusted to the tissue should be met. Further, mechanical functionality and structural integrity should be maintained for the time period that is necessary for new bone formation. Moreover, biomaterial should conform to the requirements of biocompatibility - it should promote cell attachment, spreading and proliferation of cells and facilitate the production and maintenance of extracellular matrix. Optimally, it should attract mesenchymal stem cells and promote their differentiation into osteoblasts. These objectives can be achieved by proper fitting of chemical and physical characteristics of scaffold material. The chemical characteristics include the presence of chemical groups at the surface controlling the surface energy, hydrophilicity and ability to form ionic bonds with cells [17]. The physical characteristics comprise the texture, the pore structure, size, and distribution that will allow cell and blood vessels ingrowth and the flux of nutrients. One of the biomaterials that fulfill most of the requirements are polyurethanes.
3. Polyurethanes
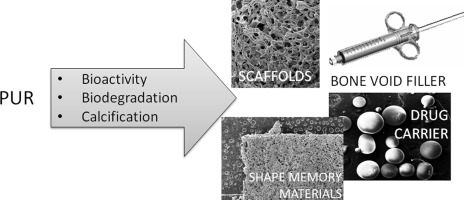
Polyurethanes (PURs) were introduced as potential biomaterials for bone and cartilage repair in the late 90's. Since then PURs were applied among others as cement, injectable void fillers, scaffolds, drug delivery systems, shape memory materials [18], [19]. PURs attract attention thanks to unique properties and chemical or physical modification possibilities. Properly designed PUR are non-toxic, biocompatible, they promote calcification in vivo [2], [3], [20], [21]. PURs have excellent mechanical and physiochemical flexibility [1]. Desirable properties of the PURs can be tailored by changing the chemical composition, the ratio of raw materials, parameters of synthesis or technology. Thus they can be obtained as stable or biodegradable, hydrophobic or hydrophilic, thermoplastic or thermosetting leading to a very broad range of products like foams, coatings, fibers or films.
3.1. How to obtain PUR? Synthesis and different components
Polyurethanes are synthesized by step growth polymerization (polyaddition) of three basic components: olygodiol (polymeric polyol), polyisocyanate (isocyanate with at least two functional groups) and a low molecular weight chain extender (diols or amines). The polyaddition can be carried out by a one-step or a two-step process.
The one-step process is mainly used in PUR foams fabrication. Water is very often used as a foaming agent, added to the reaction mixture, reacts with an isocyanate group and forms a carbamic acid derivative, which transforms into carbon dioxide after decarboxylation (Fig. 2B) and thus PUR foams can be obtained. In this method, an appropriate proportion of olygodiols, chain extender, water and other additives are mixed together with isocyanate. The isocyanate chemistry of this system is advantageous because the second product in this reaction is an amine, which reacts with remaining isocyanates resulting in urea groups. The reaction between isocyanates and amines is very fast (about 100 times faster than with diols), thus the catalyst is unnecessary. While the two-step process, also called prepolymer method is more complicated, but gives more opportunities to control synthesis parameters and parameters PUR. Moreover, a two-step process is less exothermic. In the first step of the synthesis olygodiols and excess of diisocyanates are combined to obtain a prepolymer. The prepolymer is a mixture of soft segments terminated with isocyanate groups and unreacted diisocyanates, which will form hard segments later. Thus in this step, we determine both the length of soft segments and hard segments content. In the second stage, we introduce to the reaction mixture a low molecular weight chain extender e.g. diol, diamine.
 Fig. 2. Scheme of reactions between (A) diisocyanate and olygodiol, formation of urethane group (B) isocyanate and water, formation of carbon dioxide.
Fig. 2. Scheme of reactions between (A) diisocyanate and olygodiol, formation of urethane group (B) isocyanate and water, formation of carbon dioxide.The chain extender reacts with unreacted diisocyanate to form hard segments and at the same stage, the connection between soft and hard segments also takes place. To summarize, hard segments are the reaction product of diisocyanates and a chain extender, and soft segments are a combination of diisocyanates with olygodiols. In both segments urethane groups –NHCOO- are present, but their concentration in the individual segments is different, what leads to greater or lesser rigidity of the chains. Another unique property of PUR is the separation of soft and hard segments caused by their immiscibility and interaction between the chains or the presence of hydrogen bonding. This phenomenon leads to the formation of structures called domains. The domains consist hard or soft segments. Next to domains, the structures of micrometers in size can be present in PUR as a result of agglomeration or crystallization of different chains [43], [44]. From the material science point of view, issues such as phase separation of segments into domains, nano, and micromorphology of polyurethanes are still the subject of scientific inquiry and stimulate the development of modern engineering materials.
3.2. How to control biodegradation of PUR?
One of the requirements of bone tissue engineering is that materials must be biodegradable. The degradation of PURs may be controlled by the type of olygodiol, diisocyanate and chain extender, but also, the structure (hard to soft segments ratio, the degree of crosslinking) has a dramatic effect. Properly designed PURs are biodegradable [45], [46]; they degrade mainly through hydrolytic degradation of soft segment derived from olygoesters. In the case of polyurethanes obtained from olygoethers, degradation proceeds by oxidationand subsequent hydrolysis. Hydrolysis of the hard segments is slower than the soft segments [43]. However, if groups susceptible to hydrolysis are in the hard segment, the degradation starts from those groups. In physiological conditions degradation of the urethane group is unlikely since its rate is an order of magnitude lower than the degradation rate of ester linkages. Biodegradable polyurethanes are mainly synthesized from olygoesterdiols i.e. poly(ε-caprolactone)diol (PCL), poly(glycolic acid) (PGA), poly(lactic acid) (PLA) since they are FDA (Food and Drug Administration) approved [44], [47]. Guelcher et al. [3] obtained PUR system from a novel terpolymeric composition of 60% glycolide, 30% dl-lactide, and 10% ϵ-caprolactone (PCGL) as polyol [48], LDI, pentaerythritol as a chain extender and organobismuth compound (coscat 83) as a catalyst. PUR biodegraded at a controlled rate to non-cytotoxic decomposition products in vivo, having half-lives from a few weeks to several months. Furthermore, PUR degradation products caused no pH changes in the environment as it happens when using pure polyesters like PGA, PCL, PLA, which create an acidic environment in vitro [49], [50]. Ruan et al. [42] used PLA, piperazine (PP) and HDI to obtain PUR (P-PUU, Fig. 3). The use of PP can be attractive for two reasons. Firstly, the introduction of PP improves P-PUUs hydrophilicity. Secondly, the release of alkaline PP may neutralize acidic products from the degradation of PLA diol. To ensure the growth of osteoblast cells weak alkaline pH value is required [51], [52], thus by incorporating PP as the alkaline segments, capable of neutralizing acidic products from PLA degradation, we are able to minimize accumulation of acidic products [42]. However, more research needs to be done to confirm this theory.

Fig. 3. The degradation of PLA and P-PUUs.
Reproduced with permission from Elsevier [42].Another olygodiol employed in biodegradable PURs is poly(ethylene glycol) (PEG), which possess attractive properties. This olygoether is non-toxic, soluble in water and organic solvents and it does not induce immunogenicity and antigenicity [53]. Numerous studies have shown that the addition of PEG increases the degradation rate of PURs [38], [54], [55], [56]. The PEG presence increases bulk hydrophilicity and water absorption into the material, thus enhances diffusion of water to hydrolyze the ester linkages and faster release of degradation products out of the material [57]. However, PEG speeds up degradation only in the first weeks of degradation, when water migration into PUR structure takes place [34].
The diisocyanate selection is very important as well and more complicated. The use of aromatic diisocyanates such as MDI (4,4′-methylenebis(phenyl isocyanate)) and TDI (tolylene-2,4-diisocyanate), which are widely used in the industrial application is controversial since during implantation aromatic diamines can be released. Polyurethanes synthetized from TDI or MDI degrade to the carcinogenic and mutagenic compounds - 2,4-diaminotoluene and 4,4′-methylenedianiline accordingly [58], [59]. Aliphatic or cyclic diisocyanates like 1,6-hexamethylene diisocyanate (HDI), 1,4-diisocyanatobutane (BDI), 4,4′-methylenebis(cyclohexyl isocyanate) (HMDI), isophorone diisocyanate (IPDI) have been reported to degrade to non-toxic decomposition products [60], [61], [62]. One can find in the literature the use of lysine methyl ester diisocyanate (LDI) or lysine triisocyanate (LTI). It was reported that they degrade to both acid-terminated urethane fragments and lysine, essential amino acid for humans [63], [64]. The degradation mechanism of lysine-derived isocyanates is still under investigation. Hydrolysis of urethane linkages to lysine has been reported, however, other reports showed that urethane and urea linkages are only enzymatically degraded [65], [66]. PUR from lysine isocyanates degrade faster than from other isocyanates, which has been attributed to the degradable ester linkage present in the backbone of lysine [34]. Zhang et al. [65]synthetized polyurethane foam from LDI and glycerol and investigated the degradation rate. The mass loss of PUR was about 30% after 60 days at 37 °C in aqueous solution. The degradation products were lysine, glycerol, ethanol, CO2. It should be mentioned that, in vivo, materials degrade significantly faster than in vitro due to the presence of enzymes [67]. What is more, enzymatic cleavage of the lysine molecule likely promotes the LTI scaffold degradation in vivo [66].
The third component in PUR synthesis – chain extender also allows controlling degradation rate. The conventional chain extenders used in PUR synthesis are 1,4-butanediol (BDO), m-phenylenediamine and 1,2-ethanediamine. In medical application other compounds are used as well i.e. ethylene glycol (EG), which is non-toxic and soluble in water (Table 2). It is possible to increase the degradation by introducing hydrolysable chain extenders [68] like amino acid–based diester [69], dl-lactic acid [70], ascorbic acid [71], 2,2-(methylimino)diethanol (MIDE) [29]. Those PUR undergo more rapid degradation due to the enhancement of water absorption.
Table 2. Chosen polyurethane systems used for bone repair and regeneration.
| Olygodiol | Isocyanate | Chain extender | Catalyst | Reference |
|---|---|---|---|---|
| PCL | HDI | SB | DBTDL | [17] |
| PCL | HDI | SB | – | [18] |
| PCL | HDI | SB, farnesyl, mercaptolethylether | DBTDL | [19] |
| PCL | HDI | BDO | – | [22] |
| PCL | HDI | DABCO | [23] | |
| PCL | HMDI | EG | DBTDL | [24], [25], [26], [27] |
| PCL | BDI | Tyramine | DBTDL | [28] |
| PCL | MDI | MIDE | St(Oct)2 | [29] |
| PCL, PEG | HDI | Benzoic acid | – | [30] |
| PCL, rapeseed oil | HDI | EG | – | [31] |
| PCL, DMPA, MEK | IPDI | TEA, EDA | St(Oct)2 | [32] |
| PCG, PEG | LDI | – | COSCAT 83 | [33] |
| PCGL | LTI, LDI | Pentaerythritol | St(Oct)2 | [3] |
| PCGL | LDI, LTI | TEGOAMIN 33 | [34] | |
| PCGL | HDI, LTI | St(Oct)2 | [35] | |
| PEG, PCGL | HDI trimer | TEGOAMIN 33 | [36] | |
| PEG, PCGL | LTI | TEDA | [37] | |
| PEG, PHB | HDI | DBTDL | [38] | |
| Siloxane diol | IPDI, MDI | DBTDL | [39] | |
| P(LA-pDO) | HDI | BDA, isopropanol | St(Oct)2 | [40] |
| PEA | IPDI | HDA | – | [41] |
| PLA, piperazine | HDI | Piperazine | – | [42] |
3.3. How to promote calcification of PURs?
The ideal bone graft should promote calcification of newly formed tissue in vivo. The ability to support calcium phosphate crystals formation is one of the unique properties that distinguishes PURs from other biomaterials and predisposes it for using in bone regeneration. PURs, when they are implanted into the circulatory system, within connective tissue undergo calcification [20], [21], [72]. The exact mechanism is still unrecognized, however, it is considered that it occurs by interaction of PUR with ions of calcium and phosphorus in the blood and other body fluids [73]. The determinants of calcification include factors related to host metabolism, time of implantation, the structure and chemistry of the implant [74]. The formation of CP changes in time. Firstly, amorphous calcium phosphate salts are created and then series of transformations occurs, including changing into brushite, whitlockite, octacalcium phosphate to finally form hydroxyapatite. It has been reported that, depending on the chemical composition, the calcium-to-phosphorus atomic ratio of the crystals growing on the PUR varied from 0.94 to 1.55 [20] and 1.52 to 2.0 [75].
It is presumed that the hydrophilicity and the presence of ether oxygen have the greatest impact on calcification [76]. In the case of hydrophobic polyester-urethanes calcification occurs only on the surface, which is in a direct contact with body fluids. In case of hydrophilic polyether-uretanes it occurs both on the surface and throughout the polymer. Increased calcification can be obtained by PEG modification, which will increase hydrophilicity of PUR, but also provide ether groups. Liu et al. [38] incorporated the hydrophilic PEG segments into PUR chain (PHB-HDI), thus the surface and bulk hydrophilicity were significantly improved – water contact angle decreased from 75° to 65°. The enhanced wettability resulted in nice coating with CP throughout electrospun scaffold after immersion in simulated body fluid (SBF), without any treatment. Similar results were also published by Gogolewski and Gorna [77]. They reported that newly formed cancellous bone on the scaffolds from PUR with higher content of hydrophilic component contained more bone mineral than the newly formed bone in the defects implanted with PUR with lower content of hydrophilic component. The dependency between increased hydrophilicity and scaffold mineralization was also reported by Marzec et al. [78] and Liu et al. [38].
Another way to promote calcification was reported by Aryal et al. and Tasisthat et al. [79], [80]. It was shown that carbon nanotubes with negatively charged surfaces can promote mineralization thanks to enhanced ability to nucleate hydroxyapatite (HA). Zawadzak et al. [25] have deposited carbon nanotubes by electrophoretic deposition on the surfaces of PUR scaffolds (PCL-HMDI-EG). They observed that nanotubes accelerate the precipitation of CP, due to the presence of more nucleation centers for crystal nucleation and growth, as compared to uncoated foams. It was also reported that mineralization can be increased by the addition of vitamins A and D2 to the incubation solution, in which HA-like forms grow faster [81].
In case of porous scaffolds structure and pore size also matters. Zieleniewska et al. [31] pointed out that high porosity and open-cell scaffold structure facilitate penetration of SBF (simulated body fluid) into the 3D materials, making the apatite distribution regular. The settling of phosphates is strongly affected by the extension of the scaffold surface, and any projections stimulate apatite nucleation. This statement is consistent with Schlickewei et al. [72], who showed that scaffolds with larger pores size (200–600 μm) underwent calcification, whereas no calcium deposition forms were found on the scaffolds with smaller pore sizes (140–400 μm).
3.4. How PURs interact with cells? In vitro and in vivo examination
Polyurethanes for bone tissue scaffolds are thought to be non-toxic and biocompatible. Those properties depend on the raw materials and additives used in their synthesis. Not only diisocyanate, olygodiol or chain extender is crucial as it was discussed in Section 3.2, but also type and amount of catalyst matters. Catalysts are commonly and widely used in PUR synthesis, especially tin (II) 2-ethylhexanoate (St(Oct)2), which is FDA approved, dibutyltin dilaurate (DBTDL) and 1,4-diazabicyclo[2·2·2]octane (DABCO) (Table 2). However, in the case of medical applications, the addition of catalyst is the contentious issue. On the one hand, catalysts speed up the polyurethane synthesis and increase their molecular mass, thus better mechanical properties can be obtained. On the other hand, publications from a variety of sources indicate that catalyst used in PUR synthesis can be cytotoxic. Mrówka et al. [39] investigated the influence of different catalyst: DBTDL, N-dimethylethanolamine (N-met) in poly(siloxane-urethane-ureas) synthetized from IPDI on cell viability. Also, f or comparison PUR without catalyst, synthesized from more reactive diisocyanate MDI was investigated. As measured by XTT assay (at day 7 and 21) viability of cells cultured on the surface of PUR without catalyst was very high and comparable to control culture on polystyrene. In the group of IPDI-based materials, the highest viability was found on PUR prepared using N-met catalyst. The use of a tin-containing catalyst (DBTDL) resulted in a dramatic drop of cell tolerance in direct contact in vitro. Tanzi et al. [82] investigated cytotoxic effect of different catalysts on HUVEC and 3 T3 cell lines by direct cytotoxicity test. It was shown that catalysts are cytotoxic, although to a different extents. The most toxic was DBTDL, secondly Sn(Oct)2, whereas the lowest observed cytotoxicity was induced by DABCO. High toxicity of DBTDL [83] and lack of DABCO induced cytoxicity was also reported by Moglia et al. [23]. However, in numerous studies no cytotoxicity was reported when using DBTDL [17], [19], [24], [25], [26], [27], [28], [38], [39]. One explanation may lay in the methodology, especially how the cells were exposed to the catalyst. Tanzi et al. cultured cells in solutions containing catalysts, in other studies catalysts were dispersed in PUR material, thus by the time the cells were seeded, the catalyst did not leach out and did not affect cells [82]. Therefore, contact between cells and catalyst was at a lower extent. More research needs to be done to investigate how catalyst influences cell viability, especially during long term exposition and in regard to their different content in PUR system.
Biodegradable PURs of various chemical compositions were examined in vitro and in vivo. To confirm that PUR support cell attachment, growth, proliferation and osteoblastic activity different cells line were examined: osteoblast precursor cell line MC3T3 [34], [84], human bone-derived cells (hBDC) [32], [85], human osteosarcoma cell line MG-63 [41], [86], [87] and SAOS-2 [88], and different stem cells [32], [89], [90], [91]. According to Guelcher et al. MC3T3 cells penetrated up to 5 mm into the interior of the PUR scaffold after 21 days [92] and when cultured in osteogenic medium, mineralization of ECM could be observed [3]. Another research was focused on interactions between MG-63 cells and poly(ester-urethane)urea 3D scaffold synthesized using IPDI, poly(ethylene adipate) diol (PEA) and hexamethylene diamine (HDA) as the chain extender [41]. Scaffolds were cytocompatible, supported attachment, growth and proliferation of MG-63 cells. Upon stimulation with osteogenic medium alkaline phosphatase activity reached a maximum at the 2nd week and remained at this level. SEM analysis showed CP deposits on the scaffolds seeded with cells. Researchers also studied whether PUR is appropriate material for bone regeneration by in vivo examination. PUR was implanted into critical-size segmental defects in sheep tibia [93], into the ilium of healthy [77] and estrogen-deficient sheep [94], into nude mice [91], [95], rats [36], [87]. All studies indicated that PUR are appropriate scaffold materials for bone regeneration.
As it was mentioned PURs have the unique structure (hard to soft segments ratio, the presence of the domains, various functional groups) and can be synthetized from diverse raw materials, thus, chemical, mechanical and biological properties are unique for each particular PUR system. Therefore, a series of differentiated PURs can be used as model materials to determine cell behavior on the surface with various roughness, stiffness, surface polarity, hydrophilic character etc. Bil et al. [26] have proven that the increased hard segment content influences surface properties of PUR (PCL-HMDI-EG), especially hydrophilicity, and thus, its biocompatibility. HBDC were cultured on PUR with different hard segment content ranging from 22 to 70 wt% characterized by contact angle from 94 to 71° respectively. It was proven that increasing hard to soft segment ratio resulted in the increased micro-domain phase separation on the PUR surface, thus the polar group concentration on the PUR surface and the surface hydrophilicity increased. The highest cell viability was observed on the most hydrophilic PUR, what is consistent with other publications [11], [96], [97]. However, the ALP activity decreased with the increase of hard segment content. This result was discussed in terms of different abilities of various surfaces to absorb proteins, which in turn may affect cell attachment and influence cell capability to proliferate and differentiate [96]. Kavlock et al. [28] claimed no changes in BMSC proliferation, ALP activity and mRNA level of osteopontin and osteocalcin depending on hard segments content (20–40%) of PUR composed of PCL-BDI-Tyramine. However, it is controversial to claim that hard segment content can be changed by molecular mass of olygodiol. Authors have used olygodiol in the range of 1100 to 2700 molecular weight. Calculated hard segment content is correct, but from a chemical point of view, we obtain PUR with shorter flexible segments. This modification does not lead to an increase of hard segments in the PUR structure (only higher equivalent weight), thus, experimental results may be burdened with an error. One of the methods to regenerate bone is obtaining porous materials as scaffolds. The scaffold is a 3D material to cause desirable cellular interactions to contribute to the formation of new functional tissues. This paper is describing the particular PUR systems to obtain those scaffolds.
Kommareddy et al. [11] synthesized different PURs from PTMG, HMDI, BDO and used it as a model for investigating the influence of scaffold stiffness on cell proliferation (MC3T3-E1) and bone tissue formation. On the softest PUR (74 MPa E-Modulus) the smallest number of cells adhered when compared to stiffer samples of E-Modulus 120 and 312 MPa. It indicates that material stiffness has a great impact on cell seeding and spreading. Those findings are also consistent with Mrówka et al. [39], who carried out similar research on hBDC and Page et al. [33] who studied the influence of matrix rigidity with the use of PUR films on tumor cells. Kuo et al. [32] discussed the behavior of human mesenchymal stem cells (hMSC) on electrospun PUR (PCL-IPDI-TEA/EDA) with different elasticity and on electrospun PCL scaffold. It was confirmed that the hardness could significantly influence the osteogenic differentiation of hMSCs. It appeared that PUR nanofibers with higher modulus induced more osteogenic differentiation than PCL nanofibers with the same fiber size, having lower modulus. Moreover, fibers with a smaller diameter (200–400 nm) enhanced differentiation, while those with larger diameter (600–800 nm and 1,4–1,6 μm) promoted proliferation [94].
3.5. How to enhance PURs bioactivity?
3.5.1. Incorporation of biomolecules
The incorporation of molecules in the backbone chain of the PUR may enhance its biological activity. For instance 1,4:3,6-dianhydro-d-sorbitol (SB) was introduced to the PUR structure (PCL-HDI) by Gorna et al. [17], [98]. SB and its derivatives have proven to be pharmacologically active, primarily as vasodilators [99] and an agent promoting bone formation [100]. The biological activity of this system (PCL-HDI-SB) was examined by Hofmann et al. [18]. Human bone-derived cells (hBDC) and human umbilical vein endothelial cells (HUVEC) were capable of spontaneous tissue-like organization. Immunohistochemistry and qPCR analysis of gene expression revealed stable osteoblastic and endothelial gene expression profiles. PUR synthesized from SB was also compared with PUR (PCL-HDI) manufactured with other chain extenders: bis(2-mercaptoethyl) ether and farnesyl [19]. Although SB and farnesyl modified PUR exhibited different degradation rates, hydrophilicity and mechanical properties, the in vitro and in vivo results indicated that those three PURs did not differ in terms of cell biocompatibility. Another modification was proposed by Kucinska-Lipka et al. [101] and Zhang et al. [102], who incorporated ascorbic acid (AA) into the polymer chain. PUR containing ascorbic acid had a stimulating effect on the secretion of ALP and type I collagen by mouse OPC cells, similar to the addition AA directly into the culture medium. AA was also used by Cetina-Diaz et al. [71] in PUR synthesis as chain extender with PCL as olygodiol and HMDI as diisocyanate. Biocompatibility tests showed that PUR containing AA increased osteoblasts proliferation. Thus AA modification of PUR is favorable for bone tissue repair. Further, Zhang et al. [29]proposed PUR synthesis from MDI, PCL and 2,2-(methylimino)diethanol (MIDE) as chain extender. To examine the cytocompatibility of the PURs in this study, fibroblasts were seeded on the PUR samples and compared to Tecoflex (medical grade thermoplastic polyurethane available from Thermedic) and tissue culture dishes. After 5 days of culture, fibroblasts were found to attach and proliferate on the experimental PUR. Cells cultured on porous scaffold showed superior proliferation rate in comparison to other control materials, what was discussed in terms of cell–material electrostatic interaction, chain flexibility and hydrophilicity. The tertiary nitrogen atoms in chain extender MIDE can form cationic groups, which results in slightly positive polarity. In the culture media, the polymer chains can change the conformation to form a positively charged layer on the substrate, which will interact with negatively charged cell membrane surface and most serum proteins, thus promote cell attachment and proliferation [29]. In another study carried out by Das et al. [87] vegetable-oil-based hyperbranched polyurethane PUR were blended with rapeseed protein (r-protein) functionalized multi-walled carbon nanotubes. It was reported that osteoconductivity and MG-63 cell differentiation was drastically improved. This material promoted regeneration in the tibial defect with 93% of bone regeneration only after 45 days.
3.5.2. Surface modifications
Different surface modifications are widely used to enhance cell compatibility and promote cell proliferation on PURs. Biomolecular recognition of the material by the cells can be achieved by incorporating cell-binding peptides in the form of native long chain ECM proteins, such as fibronectin, laminin, vitronectin, and collagen. Several methods have been proposed for PURs for bone tissue engineering application, such as grafting of peptides, gelatin impregnation, hyaluronic acid immobilization, wet chemical modification, gas plasma treatment [103], [104]. Among these, immobilization of collagen is the most commonly used, due to satisfying effect on cell adhesion and proliferation [105], [106]. Different approach was proposed by González-Paz et al. [86], who used chondroitin sulfate (CS), the cartilage and bone extracellular matrix component, to immobilize onto the surface of amino-functionalized PUR derived from naturally occurring oleic and 10-undecenoic acids. The immobilization of chondroitin sulfate improved the hydrophilicity. Cytotoxicity and cell morphology analysis using osteoblast cell line MG-63 showed that PUR-CS films are suitable materials for cell growth and differentiation.
3.5.3. Composites
Much work is focused on developing materials based on elastic, biodegradable PURs and their composites with bioactive ceramic fillers such as HA, β-TCP. Due to the presence of polar groups in the chain, PURs have a relatively high affinity to CP [107]. There are many ways to obtain PUR-ceramic composites among them: 1) methods based on adding ceramic before PUR polymerization: in one-step method (PUR foaming in the reaction with water) [91], [108], [109], [110], [111], [112], or in two-step method during prepolymer synthesis or before PUR gelation [113], [114], [115], [116]; 2) methods based on mixing ceramic with polymerized PUR: mixing with milled PUR [117], compressing PUR-ceramic paste [118], adding ceramic into PUR solution [119], [120], [121], [122], mixing PUR solution with HA dispersion [123], [124]; 3) ceramic immersion or impregnation on PUR surface [125], [126]. Incorporation of ceramics like HA, β-TCP or Bioglass provides osteoconductive properties and promotes bone formation. Composites production is relatively simple way to increase PUR bioactivity, especially from the industrial point of view.
3.5.4. Growth factors
To increase ostoinductive ability of PUR, it was proposed to incorporate growth factors. PUR scaffolds have been tested for controlled release of different GFs such as basic fibroblast growth factor (bFGF) [127], fluorescein isothiocyanate labelled bovine serum albumin (BSA-FITC) [128], platelet-derived growth factor (PDGF) [34], transforming growth factor beta (TGF-β) [126] and the most importantly in bone engineering morphogenetic protein 2 (BMP-2), which stimulate osteoblast differentiation and promote bone formation. First in examining PUR with encapsulated recombinant human BMP (rhBMP-2) were Li et al. [36], who worked on PUR system of PEG, PCGL-HDI trimer. Group investigated the effects of different rhBMP-2 release strategies on new bone formation in PUR scaffolds synthesized from PCLG, PEG and HDI trimer, implanted in rat femoral plug defects (Fig. 4). The material supported ingrowth of the new bone only after 2 weeks. The addition of rhBMP-2 as a dry powder into the foaming reaction promoted bone formation more extensively than the addition of rhBMP-2 encapsulated in PLGA microspheres. The investigation of different rhBMP-2 release strategies was also carried out by Kim et al. [129]. The sustained release of the rhBMP-2 from LTI/PEG-based PUR scaffolds was shown for 21 days. The bioactivity of the rhBMP-2 containing releasates was determined using hMSCs and compared with exogenous rhBMP-2 (positive control). Although, ALP activity of hMSCs was lower, the mineralization at 14th day was significantly higher in the scaffolds than in the positive control. Other work described fabrication method of PUR membrane (PUR system information not provided) with a controllable amount of acidic fibroblast GF by layer-by-layer assembly technique [130]. Slow release of GF up to 8 days was shown, and it affected the attachement and proliferation of hMSC. Similar results were reported by Hsu et al. [131], who examined rhBMP-2 incorporated into commercially available PUR Nesopore in nasal bone defect in rabbits and others [132], [133].

Fig. 4. In vivo evaluation of the effects of PUR/rhBMP-2 scaffolds on new bone formation in a rat femoral plug model. The PUR were implanted into rat femoral plug defects (A), and harvested for μCT imaging at weeks 2 (B) and 4 (C) respectively. Treatment groups included: PUR control (no rhBMP-2), PUR/rhBMP-2, PUR/PLGA-L-rhBMP-2, and PUR/PLGA-S-rhBMP-2.
Reproduced with the permission from Elsevier [36].4. PUR applications in bone regeneration
Commercially available products for bone repair offered by the very top 3 companies in the world, are 1) metals and stable polymers like UHMWPE, PMMA, PEEK, however the publication focuses on biodegradable biomaterials, 2) calcium phosphates: β-TCP (ChronOS®, DePuy), β-TCP and dicalcium phosphate anhydrous (HydroSet™, Stryker), β-TCP and BioactiveGlass (Vitoss®, Stryker), 3) biodegradable polymers: PLGA (RapidSorb®, DePuy), 4) calcium phosphates with polymers: PLGA and calcium phosphate (Norian®, DePuy), PLLA and HA (BIOSURE™, Smith & Nephew), PLGA and β-TCP and calcium sulfate (REGENESORB, Smith & Nephew). The advantages of polyurethanes over them, were presented in 2. Polyurethanes. To summarize, PUR degradation products caused no pH changes in the environment as it happens when using pure polyesters (like PGA, PCL, PLA), PURs undergo calcification in vivo (are able to support calcium phosphate crystals formation), PURs can be foamed in situ by carbon dioxide released. Moreover, PURs can be easily proceeded due to unique chemical or physical modification possibilities, what is an huge advantage over ceramics. The calcium phosphates like HA, β-TCP are too fragile to be used as bone scaffolds alone, thus commercially are available as bone grafts. Main problem with grafts is to provide an intimate contact with the bone edges. The increased contact between material and bone promote cell migration, and might help to eliminate shear forces at the bone-implant interface, thus improve bone healing. In case of rigid materials like ceramics, it is possible to enhance fibrin-clotting on the material by for example coating with fibrinogen, what enables the migration of host cells into the implanted material. However, for elastomers such as PURs, this modification is redundant. Grafts from PUR elastomers placed in the tissues undergo swelling by absorbing body fluids. The swelling causes expansion of its volume, what also increase direct contact between the material and the host tissue [41]. It is worth noting, that in the case of polymer-ceramic composites PURs have a huge advantage over other polymers, (as it was described in Section 3.5 How to enhance PURs bioactivity? Composites) due to the presence of polar groups in the chain, PURs have a relatively high affinity to calcium phosphates.
4.1. Bone void fillers
Bone void filler (BVF) is a reactive liquid that subsequently cures to form a solid graft with bone-like mechanical properties [134]. PUR implanted in bone defects in vivo generated a minimal inflammatory response, and supported cell growth and bone regeneration [37], [94], [108], [118], [122]. Polyurethane resin obtained from fatty acids extracted from Riccinuscommunis (trade name COR – Composto Oleo de Ricino) was implanted into rabbit's bone defect [135]. No inflammatory foreign body reaction was observed after 3 months, and a connection between the PUR - bone surface and presence of a thin layer of newly formed bone was reported. Lysine-derived polyurethane PUR - allograft composite was also used as BVF [111], [136]. It was reported that osteoclasts infiltrated the material along the surface of the mineralized particles and osteoblasts subsequently deposited new matrix. Interestingly, it was shown that the size, not a number of allograft particles in the composite regulates regeneration process. Void treated with composite having small particles (up to 100 μm) healed partially after 12 weeks, irrespective of the allograft amount, while composite with particles in the range of 100–500 μm healed bone completely [137]. These results confirm that PUR is a good bone substitute for use in the repair for great bone losses.
However, in situ forming scaffolds can better fill irregularly shaped defects, improve the connection with surrounding tissue and eliminate shear forces [138]. Thus, a biodegradable and porous scaffold that can be injected into the defect and foamed at body temperature can potentially improve tissue regeneration. Thermoplasts cannot be injected, but melted or dissolved ex vivo before implantation to form a scaffold. Hydrogels are injectable and many of them support cell growth and proliferation such as PEG, collagen, chitosan, alginate and hyaluronan. However, mechanical properties of hydrogels are inappropriate for bone tissue engineering. What is more, hydrogel scaffolds have 10–100 nm pore sizes, what limits cell migration [139]. PUR foaming in situ by carbon dioxide released in the reaction of isocyanate with water seems to be a perfect way to obtain injectable scaffold. In Fig. 4 injectability of PUR scaffold is shown. Scaffolds obtained by Hafeman et al. [34] from PCGL, LDI and TEGOAMIN 33 as a catalyst, gelled after 5 min and the temperature of the foaming did not excite 40 °C, thus,this system can be applied as BVF (Fig. 5). Other, two-component injectable PUR systems have been safely impranted in animals without serious adverse reactions [37], [136], [140], [141].

Fig. 5. Injectability of PUR scaffolds: time-lapse photographs showing an injection of the reactive liquid system.