1. Introduction
Researchers have made countless advances in developing and testing drugs to combat deadly diseases. However, the completion and approval of a drug takes approximately 12 years, which can sometimes cost millions of lives [1]. Additionally, using two-dimensional (2D) cell culture models and animal models during the preclinical testing phase of new drugs has led to a low approval rate during the last decade [2], [3]. The failure of 2D cell cultures to predict the effects of drugs accurately is primarily due to the lack of similarity between these cultures and a three-dimensional (3D) microenvironment and its static culture conditions, and animal models are comparably expensive and anatomically different from the human body. Therefore, new in vitro cell culture methods have recently been developed to achieve adequate and efficient tests [4], [5].
On the one hand, research on organ-on-a-chip technology has pushed cell culture methods toward greater accuracy. Generally, an organ-on-a-chip can be defined as a microfluidic device containing organ-specific cells and simulating organ-level functions. It is also a useful tool that can be easily controlled, analyzed, and most importantly, can mimic complex tissues in a miniaturized volume. This new approach, which arguably has more advantages than the traditional 2D monolayer static cell culture method, has proved to be a better alternative to animal models in terms of its capacity to culture human tissues, cost, and ethical and public concerns [6]. The feasibility of the organ-on-a-chip device is another major incentive that has pushed researchers to apply it to mimic several human organs such as the heart [7], [8], [9], [10], lung [11], [12], [13], liver [14], [15], [16], skin [17], [18], [19], brain [20], [21], [22], and kidneys[23], [24].
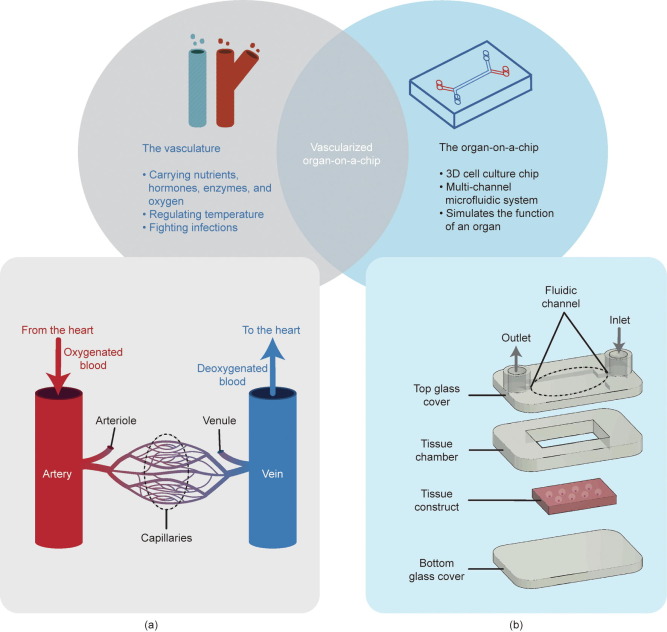
On the other hand, mimicking an in vivo organ requires detailed knowledge of its functions. The most abundant organ in the human body is the vascular system, a circulatory system of vessels carrying oxygen and nutrients to other body systems, including the respiratory system, the digestive system, the kidneys, and the urinary system. Accordingly, the vasculature plays an essential and critical role in maintaining the body in a steady-state and ensuring optimal organ function. Thus, integrating a system of nutrient and oxygen supply, in other words, the vasculature, into organs-on-a-chip is necessary to recreate the microenvironment and physiological functions of the organ (Fig. 1).
 Fig. 1. Main functions of the vasculature and an organ-on-a-chip, and their intersection on a vascularized organ-on-a-chip. (a) Schematic of a circulatory system including capillaries and blood flow; (b) basic structure and compounds of an organ-on-a-chip.
Fig. 1. Main functions of the vasculature and an organ-on-a-chip, and their intersection on a vascularized organ-on-a-chip. (a) Schematic of a circulatory system including capillaries and blood flow; (b) basic structure and compounds of an organ-on-a-chip.In this review, we focus on the construction of a vascularized organ-on-a-chip device. First, the vasculature and organ-on-a-chip fabrication process is described with particular attention to two critical steps: chip structure manufacture and tissue construction. The importance of applying vasculature on several organ-on-a-chip and tumor-on-a-chip devices will be demonstrated by describing various recent and highly accurate models, which would help identify a new, promising avenue for drug screening.
2. Fabrication of the vascularized organ-on-a-chip
Organs-on-a-chip and vascularized organs-on-a-chip have been fabricated using several innovative methods [25]. These approaches substantially vary based on the targeted characteristics to be achieved in the model. Generally, the fabrication of an organ-on-a-chip device is completed in five steps (Fig. 2). The first step is the designing of the organ-on-a-chip platform and modeling it in 3D. The next step is to manufacture the structure of the device using either lithography-based methods or other methods that allow the use of a compatible material. After manufacturing the device, tissue construction is generally achieved using a microfluidic or bioprinting strategy. The organ-on-a-chip is typically composed of several layers because of the complexity of the tissue and the structure of the device; moreover, the microfabrication method has limitations in the second step of the process, which requires a bonding step to connect all the parts and form the chip. The device is then connected to a fluid circulatory system that carries nutrients or drugs, allowing precise control of the entire system. In some relevant studies [26], [27], [28], fabrication was achieved in only three steps by completing the device and tissue fabrication in a single step using a bioprinting technique that does not require bonding. Finally, fabrication of the platform structure and bioprinting of the tissues, the most challenging and vital steps, especially in the creation of vascularized tissues for organs-on-chips, are achieved; we have described them in detail.
 Fig. 2. The fabrication process of an organ-on-a-chip device.
Fig. 2. The fabrication process of an organ-on-a-chip device.2.1. Designing the organ-on-a-chip platform
The first is a prefabrication step, which consists of designing the device and modeling it in 3D, including the cover, tissue chambers, tissue constructs, and fluidic channels, using computer-aided design. This is subsequently transformed into a standard triangle language file when a 3D printing strategy is chosen. Notably, for the construction of a vascularized organ-on-a-chip, this step requires additional modeling of the vasculature [29]. Therefore, a prelaminar study to choose the appropriate vasculature model is of utmost importance. The vasculature model is chosen based on the targets of the project, such as geometrical complexity or high functional efficiency of the vasculature. Because the current advances in vasculature models have still not led to a complete model, the choice of a suitable model brings into play the advantages and disadvantages of different biofabrication methods, which will be described later in this paper.
2.2. Manufacturing the device structure
Currently, microfabrication methods are intensely being developed using a wide variety of techniques described in the literature. Therefore, the following section will focus on newly developed methods, the most commonly used lithography-based methods, (including soft-lithography and photolithographymethods), and other non-lithographic methods.
2.2.1. Soft-lithography method
Soft lithography is a method widely used to replicate a structure using a prefabricated mold [30]. The “soft” in the name comes from the elastomeric nature of the material. Polydimethylsiloxane (PDMS) is generally considered the most suitable material for this method. The main advantages of soft lithographyare its high micro-size precision and cost-effectiveness. It involves replica molding (REM), microcontact printing, micro-molding in microcapillaries, micro-transfer molding, and solvent-assisted micro-molding.
In general, REM is the most popular soft-lithography method. The REM method starts with constructing a master mold that will be used for a secondary cross-linkable material. After this material is molded, the mold is detached, followed by replication in the reverse mode [31]. The same process was used by Zheng et al. [32] to create micro-vessels on a chip, enabling the study of angiogenic activities and the thrombotic nature of endothelialized microfluidic vessels. Additionally, Miali et al. [33] proved the versatility of this method, that is, the REM process was used to create authentically complex microvasculature networks inspired by a Hedera elix leaf. Freshly collected leaves were taped to obtain a negative print in a PDMS mold. Next, the replica was used to create a SU8-5 template and achieve a sandwiched system mimicking the complex geometrical and biological properties of the human vasculature.
Similarly, Nie et al. [34] considered the complex structure of a real in vivovascular network as a target to mimic. They chose to proceed at three different levels (Fig. 3(a)) [34]. First, to manufacture a high-resolution template, 3D printing was integrated into the process. A classic casting, peeling, and bonding process was used, but interestingly was combined with a dual crosslinking strategy to obtain a hollowed platform allowing the final step, specific cell loading.
 Fig. 3. Microfabrication methods of vascularized platforms. (a) Soft-lithography method: the fabrication process of a multiscale vascular chip using 3D printing and dual-crosslinking techniques. GelMA: gelatin-methacryloyl. (b) Photolithography method: a new photolithography technique is shown on the left and on the right is the standard photolithography technique. (c) Non-lithographic method: the SMART process was used to fabricate a microchannel. PC: polycarbonate. 1 bar = 105 Pa. (a) Reproduced from Ref. [34] with permission of the Royal Society of Chemistry, ©2020; (b) reproduced from Ref. [38] with permission of the Royal Society of Chemistry, ©2019; (c) reproduced from Ref. [39] with permission of Wiley-VCH Verlag GmbH and Company KGaA, ©2018.
Fig. 3. Microfabrication methods of vascularized platforms. (a) Soft-lithography method: the fabrication process of a multiscale vascular chip using 3D printing and dual-crosslinking techniques. GelMA: gelatin-methacryloyl. (b) Photolithography method: a new photolithography technique is shown on the left and on the right is the standard photolithography technique. (c) Non-lithographic method: the SMART process was used to fabricate a microchannel. PC: polycarbonate. 1 bar = 105 Pa. (a) Reproduced from Ref. [34] with permission of the Royal Society of Chemistry, ©2020; (b) reproduced from Ref. [38] with permission of the Royal Society of Chemistry, ©2019; (c) reproduced from Ref. [39] with permission of Wiley-VCH Verlag GmbH and Company KGaA, ©2018.2.2.2. Photolithography method
Photolithography (also known as optical lithography or ultraviolet (UV) lithography) is based on transferring parts from a mask to a bulk or thin film[35], [36], [37]. This technology enables high precision within a range of a few nanometers and allows the fabrication of comparatively complex structures, making it an accurate and powerful tool to construct vasculature-like microchannels. However, this is a time-consuming and relatively expensive method. In a recent study, Fenech et al. [38] proposed a new photolithography-based technique to fabricate a vasculature that was geometrically close to real natural vasculatures. The process was based on using backside illumination and an optical diffuser to create a SU-8 photoresist mold, which has controllable rounded sections and direct proportionality between height and width (Fig. 3(b)) [38].
2.2.3. Non-lithographic method
Although lithography-based methods have several limitations, researchers have never stopped improving them and proposing solutions to overcome these problems. One of the most frequently encountered limitations in the microfabrication of an in vitro vasculature is recreating a rounded cross-section, which motivated Kappings et al. [39] to develop a new technology called vasQchip. Generally, to simplify an element of a machine function, it is advisable to look for its symmetries. Thus, the same reasoning could be applied to the tubular geometry of the real vasculature to create a simplified model. In the same study, the research team constructed a semicircular scaffold with a porous microchannel. The fabrication process of the channels was called substrate modification and replication by thermoforming (SMART) technology. It begins with irradiation of a polycarbonate film with heavy ions and then using the micro-thermoforming process to create a semicircular form to bond the microchannel (Fig. 3(c)) [39]. However, no recent studies have demonstrated the ability to fabricate a multiscale and ubiquitous vasculature structure using the SMART technology.
2.3. Constructing the vascularized tissues
Three models of constructing vascularized tissues have been proposed by several research teams during the last decade, including the endothelial barrier-based model and the vascular formation-based model (the angiogenesis and vasculogenesis models) (Fig. 4) [40], [41]. The endothelial barrier model involves creating a 3D structure by patterning endothelial cells (ECs) on an organ-on-a-chip device wall [42], [43], [44], [45], [46], [47]. Generally, this model is selected for its feasibility and controllability, although it is not reliable for mimicking angiogenesis and vasculogenesis. The vasculogenesis model is based on the differentiation of ECs with de novo vascular network formation. The angiogenesis model is constructed by growing and sprouting new capillaries from existing blood vessels [48], [49], [50], [51], [52], [53], [54], [55]. More importantly, synergy between the endothelial barrier-based model and the vascular formation-based model was achieved by Wang et al. [54] to create a device allowing a tight connection between the artery/vein and the capillary networks, which could also be an efficient tool for interconnecting several organ tissues and to create a body-on-a-chip platform.
 Fig. 4. Schematic of the vasculature models, including the endothelial barrier model, the vasculogenesis model, and the angiogenesis model [40], [41].
Fig. 4. Schematic of the vasculature models, including the endothelial barrier model, the vasculogenesis model, and the angiogenesis model [40], [41].After choosing the vasculature model, one must select a fabrication strategy for the microvasculature and organ tissues. Two main strategies exist: the microfluidic strategy, which uses the micromechanical and biochemicalbehavior of targeted cells under well-defined microfluidic conditions to control their positioning in the device; and the bioprinting strategy, which is based on direct cell or tissue deposition.
2.3.1. Microfluidic strategy
Integrating ECs in an organ-on-a-chip device is fundamental to ensuring vascular–organ interactions. Microfluidic physics is the oldest most widely used method for controlling cells in microphysiological systems. The microfluidic strategy involves applying microfluidic pressure on perfused cells to encapsulate them under certain structural and functional conditions. There are two main microfluidic methods, namely the wall-trapping method and the microencapsulation method (also known as the self-assembly method).
2.3.1.1. Wall-trapping method
Recreating vasculature in an organ-on-a-chip device can be realized by trapping ECs in a wall. The wall-trapping method is adequate for constructing endothelial barrier-based models. This method is based on perfusing cells through microfluidic channels that contain a porous membrane, an extracellular matrix (ECM), or a hydrogel. The seeded cells are then fixed in the sidewall of the channels to form an endothelial barrier.
If a porous membrane is used, it is constructed using the microfabrication techniques described previously, and generally, PDMS is regarded as a suitable choice for the membrane material. Indeed, the membrane can culture more than one type of cell. Therefore, it can be used to study cell–cell interactions, although full contact between both sides of the cell cannot be assured because they are partially covered with the membrane. Similarly, van Engeland et al. [56] considered the membrane as an internal elastic lamina and co-cultured ECs on the upper side of the microfluidic and vascular smooth muscle cells (VSMCs) on the other side. The elastic properties of PDMS allowed the examination of the EC-VSMC interaction and signaling under hemodynamic conditions, as well as in different mechanical stretching and relaxation states of the membrane. Questioning the optimality of the dimensions and number of pores in the membrane is essential for designing porous membranes. Pore size has a direct influence on permeability and nanoparticle transmigration. Thus, it affects drug migration and other biological phenomena, such as tumor metastasis [57]. Overall, however, the wall-trapping method based on a porous membrane faces a marked limitation because the membranes are generally planar and lack the hollowed aspect of in vivo vasculature.
Another option besides a porous membrane is a hydrogel to trap seeded cells. Generally, a collagen or fibrin gel is chosen to create an endothelial wall, which can be constructed using an ECM gel. The use of hydrogels is advantageous for creating lumenized channels. Although the fabrication of a hollowed structure remains challenging without resorting to bioprinting methods, a tubular object such as a needle can be used as a pattern to be removed later in the process after crosslinking the hydrogel [58]. Additionally, the hydrogel-based wall-trapping method allowed full interaction with the surrounding cells without utilizing an intermediate membrane. Although the wall-trapping method is primarily used in the endothelial barrier model, Pauty et al. [59] were able to use it for the angiogenesis model. The research team used a PDMS chip to support the collagen gel, where a bovine serum albumin (BSA)-coated acupuncture needle was inserted and withdrawn to generate a hollowed microchannel structure. Human umbilical vein endothelial cells (HUVECs) were injected and trapped in the microchannel walls. Next, using vascular growth factors, sprouting was induced from the initial vascularized microchannels. This method has been demonstrated to be an efficient tool for studying antiangiogenic drugs, in addition to testing angiogenesis and the permeability of the vascular structure.
Finally, the wall-trapping method can be considered a rapid option to recreate planar or hollow vasculature in vitro, using an elastic membrane or a hydrogel to trap the ECs. However, current methods for hollowing the supporting hydrogel are not accurate and cannot overcome precise geometric and dimensional constraints. Moreover, the cell seeding process generates high shear stress, which harms the trapped cells.
2.3.1.2. Microencapsulation method
Using microfluidic chambers or microchannels to encapsulate ECs under morphogenetic conditions is another method used to recreate the vasculature without applying high shear stress on the cells. The chamber encapsulationmethod is generally referred to as the self-assembling or self-morphogenesis method because the encapsulated cells spontaneously start forming vasculature under precisely well-defined microenvironmental conditions. Therefore, the current method is adequate for producing vasculogenesis and angiogenesis models.
Generally, cell microencapsulation is followed by the injection of a growth factor to promote vascular sprouting and formation. Vascular endothelial growth factors (VEGFs) are broadly used in this method, as well as a few other factors, including fibroblast growth factors (FGFs). FGFs not only exert an effect on blood vessel formation, but also on all other cell types that are important for the formation of arterial vessels [60]. Nevertheless, FGFs are still not well evaluated and are rarely used in vascularized organs-on-chips. Angiopoietins(ANGs) are also added to stabilize (ANG-1) or destabilize (ANG-2) the vascular structure. Campisi et al. [61] cultured human induced pluripotent stem cell-derived endothelial cells (iPSC-ECs) in a microfluidic device. The device was supplemented with VEGF, leading to the successful creation of a vascularized network and an effective platform allowing the tri-culture of iPSC-ECs, pericytes, and astrocytes to mimic the complex structure and microenvironment of the blood–brain barrier (BBB). The encapsulation of ECs under morphogenetic conditions usually generates ubiquitous vascular networks with unexpected sprouting patterns, which is a substantial disadvantage for constructing an organ-on-a-chip intended to imitate precise and accurate tissue structure and function. Several attempts to achieve a controllable vasculogenesis direction have been conducted and realized by applying microfluidic forces. More precisely, three main forces are involved in shaping the newly formed vasculature by controlling the radius, length, and thickness of microvessels. These forces include shear stress, which is parallel to the tissue surface and is induced by flow characteristics, such as the viscosity and velocity of the perfused fluid, circumferential stress tangential to the tissue surface, and axial stress, which is generated by intraluminal pressure [62]. In addition to the biomechanical factors, many other undefined factors can influence the shapes produced by vasculogenesis and angiogenesis; thus, the morphogenetic factors are still not considered efficient tools for recreating an exact structure.
2.3.2. Bioprinting strategy
Deposition of tissues are generally realized by an emerging biofabrication technique called bioprinting, a newly developed additive manufacturing process that adds biomaterials layer by layer in different ways [63]. The main advantage of bioprinting is its cost-effectiveness and versatility; it is also considered a time-saving technology [64], [65]. Therefore, using this technology makes it possible to recreate the ubiquitous 3D structure of the entire vascular network. Bioprinting is a polyvalent strategy that allows the efficient construction of the three previously mentioned models. Indeed, five bioprinting methodologies currently exist, and each has its constraints and applications (Fig. 5).
 Fig. 5. Schematic of different 3D bioprinting methods. DMD: digital micromirror device.
Fig. 5. Schematic of different 3D bioprinting methods. DMD: digital micromirror device.2.3.2.1. Inkjet-assisted bioprinting
Inkjet technology is a drop-on-demand (DOD) process based on actuating a nozzle with heat or piezoelectricity to put droplets on a stage controlled in 3D. Inkjet bioprinting is usually used because it is a cost-effective method and can maintain high cell viability due to the low shear stress applied on cells (a consequence of the low viscosity-materials used, such as fibrin and collagen) [66]. Nevertheless, this method has low precision and structural integrity. Although droplet-based bioprinting methods are generally inadequate for manufacturing a vertical structure, Hewes et al. [67] successfully achieved a free-standing vasculature in a fibrin matrix using a piezoelectric nozzle. However, the inkjet bioprinting method is not suitable for biofabricating the vasculature because of the need for high structural stability and complexity. Thus, very few inkjet-bioprinted vascularized in vitro models can be found in the literature.
2.3.2.2. Laser-assisted bioprinting
To achieve high-speed and high-resolution bioprinting, researchers [68], [69], [70] have developed another DOD method, a laser-assisted method in which an energy-absorbing layer carries a layer of the printed biomaterial to be irradiated by a laser source to construct the desired structures. However, the laser-assisted method is not broadly used compared to other bioprinting methods owing to its low structural integrity and scalability and the limited options for adequate biomaterials. This method is generally applied to 2D cell printing; thus, DOD methods are commonly excluded when a vascularized tissue is bio-fabricated. Nevertheless, in a fascinating study, Xiong et al. [71] demonstrated the versatility of this method by creating a freeform bifurcated tubular structure that could potentially serve as a structure for in vitro vascular networks.
2.3.2.3. Micro-extrusion bioprinting
The micro-extrusion method is based on pushing the biomaterial through a nozzle under compression. This pressure can be either pneumatic or mechanical [70], [71], [72], [73], [74]. The micro-extrusion method is characterized by continuous deposition, feasibility, and good compatibility with several biomaterials. Finally, choosing this method comes at the cost of high shear stress applied to the cells. The flexibility of micro-extrusion-based bioprinting is evident in its ease of integration into the production process, from printing a single part of the microchip device to a complicated system. Lee and Cho [27] created one of the first one-step fabrication strategies to manufacture a liver with a planar endothelial barrier. The choice of printing material is a crucial initial step; therefore, PDMS was compared to poly(ε-caprolactone) (PCL) on two levels. The team found that the hydrophobicity of both materials was almost equal when measuring their contact angle side by side with a water droplet. The second level was protein adsorption, which generally seems to be neglected, although it is essential in maintaining the medium composition in an “on-chip” device. PCL has comparably low protein absorption, making it more suitable for this type of application, regardless of its low optical transparency. The one-step fabrication method enables spatial heterogeneity and does not require a secondary cell-seeding process as in stereolithography (SLA)-based fabrication methods.
As in standard micro-extrusion bioprinting, embedded bioprinting is an extrusion-based method that uses a supporting material to stabilize the extruded structure and counteract the gravitation to construct spatially complex architectures. Bhattacharjee et al. [75] used a granular gel as a bioprinting medium, with a tip injected to trace the spatial path of the microvasculature. After injection, the support material was rapidly solidified to trap the embedded material. Many materials, such as silicones, hydrogels, colloids, and living cells, can be injected using this approach; it is also considered one of the most structurally stable biofabrication methods. The classical embedded bioprinting method is a new embedded method that takes advantage of the structural stability of the classical method and creates a freeform structure with a reversible supporting material [76]. This method is called the freeform reversible method or simply the FRESH bioprinting method, and consists of bioprinting tissues in a specifically chosen temporary, thermoreversible, and washable support. After washing the supporting material, a highly complex and stable structure is obtained. The FRESH bioprinting method is thus regarded as an acceptable and advantageous method for constructing a ubiquitous structure of vasculature [77].
2.3.2.4. Stereolithography bioprinting
SLA is a photocuring-based strategy that was first proposed in 1986, which means that it is one of the earliest bioprinting methods [78]. The process begins by selecting a UV-curable material that will later be crosslinking layer by layer [79]. The traditional SLA method provides higher precision and accuracy than other bioprinting methods, but it is also time-consuming because it is based on point-by-point photopolymerization. A recent derivative form of SLA is digital micromirror device (DMD) SLA bioprinting, also known as digital light printing (DLP), which offers higher precision. Indeed, unlike standard SLA, which uses a single mirror, the DMD generally has thousands of adjustable mirrors, allowing better flexibility. Both methods are high-resolution bioprinting modalities and more expensive than other methods. Bioink is another critical choice because of the limited options available in the current literature. Zhang and Larsen [80]adopted poly(ethylene glycol) diacrylate (PEGDA, MW 700) to fabricate a perfusable vascular network. The platform was quite structurally stable, with a perfusion lifetime of at least seven days. Another fascinating and recent study by Grigoryan et al. [81] using DLP proved the complex structure biofabrication potential of this method, for creating 3D intravascular topologies and multivascular networks. The research team achieved a monolithic lung-mimetic perfusion system inspired by the alveolar sac, which is surrounded by a fully functional vascular network, to demonstrate the integrity of the proposed technology. The hydrogel used was a mixture of PEGDA and gelatin-methacryloyl (GelMA) obtained from an optimized passive micromixer. This approach can be regarded as a revolutionary method for constructing vascularized organs-on-chips.
2.3.2.5. Sacrificial bioprinting
Another bioprinting approach, sacrificial bioprinting, can be considered an indirect bioprinting method because of the need for a post-bioprinting technique to remove the fugitive bioink that is was initially directly printed, followed by a different hydrogel matrix that supports the structure [82], [83]. The sacrificial bioprinting method is an ideal method for constructing lumenized vascular networks [63]. Ji et al. [84] proposed a novel modified bioprinting approach that combines the application of a photocurable hydrogel with the sacrificial bioprinting method. Photocuring was carried out throughout the process by partially curing a freshly printed layer and executing full curing immediately after achieving the direct printing of the platform that would later be immersed in phosphate-buffered saline (PBS) to dissolve the sacrificial material. This approach slightly affects cell viability and enhances and strengthens the mechanical properties to produce a robust platform.
These various bioprinting methods have their advantages and disadvantages (Table 1) [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82] and have been continuously explored and developed. The choice of a suitable method for the targeted organ-on-a-chip model depends on several parameters, including the cell types, tissue structure, and most importantly, the primary functions of the organs. Understanding the fabrication process of a vascularized organ-on-a-chip is insufficient for perceiving its integrity using the targeted organ model. Studies have aimed at the biofabrication of human tissues and organs differently owing to the particularity and distinctiveness of each of the functions and structure of the organs. Therefore, considering the critical role that the vasculature plays in real organs and tumor growth, selecting a suitable biofabrication process for a vascularized organ/tumor-on-a-chip is complicated. The only way to attain a thorough understanding of how to construct an efficient model is to review different methods that have been integrated for each specific organ model. Thus, it is necessary to highlight recent developments that have been achieved in vascularized organs-on-chips.
Table 1. Advantages and disadvantages of various bioprinting methods.
| Bioprinting techniques | Advantages | Disadvantages | Refs. |
|---|---|---|---|
| Inkjet-assisted bioprinting | Medium resolution, medium accuracy, rapid, low cost | Requires low-viscosity materials, low structural integrity, inferior mechanical properties, nozzle clogging | [64], [65] |
| Laser-assisted bioprinting | Medium resolution, wide range of printable materials, high accuracy, high cell density, nozzle free | Low structural integrity, inferior mechanical properties, heat harms cells, time-consuming, high cost | [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79] |
| Micro-extrusion bioprinting | Superior mechanical properties, wide range of printable materials, high cell density, rapid, medium cost | High shear stress, low resolution, low accuracy, nozzle clogging | [70], [71], [72], [73], [74], [75] |
| Stereolithography bioprinting | High resolution, high accuracy, no shear stress, nozzle free | Limited range of materials, ultraviolet radiation harms cells, time-consuming, high cost | [76], [77], [78], [79] |
| Sacrificial bioprinting | High structural integrity, superior mechanical properties, adequate for hollowed constructs, medium cost | Long fabrication process, low resolution, low accuracy | [80], [81], [82] |
3. Reproducing the vasculature in organs- and tumors-on-chips
3.1. Organs-on-chips
The recreation of vasculature in vitro is critical for constructing in vivo-like organs because the vasculature plays a vital role in maintaining the properties and functions of tissues. Vascularized in vitro organs have been achieved for several organs-on-chips, but most importantly for the lung, liver, skin, heart, BBB, and kidney.
3.1.1. Lung
The lung is the primary source of oxygen in the human body; it exchanges gas between the environment and the inner vascular system based on the continuous dynamic movement of the diaphragm. Deep in the lungs, the pulmonary alveoli are found at the bronchioles, where they perform the critical function of gas exchange. During pulmonary alveolar expansion, a fragile layer of alveolar epithelial cells facing the inhaled air allows dioxygen passage to the ECs and then to the capillaries. During exhalation, carbon dioxide is expelled.
The earliest on-chip model was a lung-on-a-chip model developed by Huh et al. [85]. The device could co-culture different cells and mimic the mechanical expansion and contraction of the alveoli (Fig. 6(a)) [85]. The device comprised a porous membrane coated on both sides; by ECs on the upper side and by alveolar epithelial cells on the lower side. The vascularization model is an endothelial barrier model that uses the cell seeding method on a porous membrane. Simultaneously, the chip was used to simulate drug toxicity-induced pulmonary edema with breathing-like motion. In another study, vascularization was demonstrated to be achievable in a lung-on-a-chip using cell seeding on an ECM wall (Fig. 6(b)) [86]. Zhang et al. [86] fabricated a microfluidic device containing three microchannels that supported the alveolar epithelial cells, ECM, and HUVECs. On the side of the lung containing the epithelial cells, TiO2 and ZnO nanoparticles were perfused to test their toxic effects on the vascularized lung model. The ECM-based cell seeding method provided better cell–cell and cell–matrix interactions than the membrane-based cell seeding method; however, the membrane-based method showed great potential for recreating the mechanical dynamics of an actual lung.
 Fig. 6. Vascularized organs-on-chips. (a) Schematic of the dynamic lung-on-a-chip. (b) Schematic of a lung-on-a-chip utilizing an ECM wall. NPs: nanoparticles. (c) A liver-on-a-chip model supporting the liver microenvironment and biliary system. dECM: decellularized ECM. (d) Schematic of a one-step fabricated liver-on-a-chip. (e) Schematic of angiogenesis-based vascularization in a skin-on-a-chip, which included endothelial growth medium (EGM), human dermal fibroblasts (HDFs), keratinocytes (KCs), and an EpiLife medium [90]. (f) Vascularized skin-on-a-chip containing HaCaT cells, ECs, and fibroblasts [19]. (g) Schematic of a heart-on-a-chip supporting valvular endothelial and interstitial cells separated by a porous membrane. (h) Schematic of the co-culturing BBB model with human brain vascular pericytes(HBVPs), HBMECs, and HAs [93]. (i) Layout of a neurovascular unit [94]. (j) Schematic of renal organoid on-chip with a representation of the formation of the vascularized organoid. PSCs: pluripotent stem cells [97]. (a) Reproduced from Ref. [85] with permission of the American Association for the Advancement of Science, ©2012; (b) reproduced from Ref. [86] with permission of the Royal Society of Chemistry, ©2018; (c) reproduced from Ref. [88] with permission of IOP Publishing Limited, ©2019; (d) reproduced from Ref. [27]with permission of the Royal Society of Chemistry, ©2016; (g) reproduced from Ref. [92] with permission of the Royal Society of Chemistry, ©2013.
Fig. 6. Vascularized organs-on-chips. (a) Schematic of the dynamic lung-on-a-chip. (b) Schematic of a lung-on-a-chip utilizing an ECM wall. NPs: nanoparticles. (c) A liver-on-a-chip model supporting the liver microenvironment and biliary system. dECM: decellularized ECM. (d) Schematic of a one-step fabricated liver-on-a-chip. (e) Schematic of angiogenesis-based vascularization in a skin-on-a-chip, which included endothelial growth medium (EGM), human dermal fibroblasts (HDFs), keratinocytes (KCs), and an EpiLife medium [90]. (f) Vascularized skin-on-a-chip containing HaCaT cells, ECs, and fibroblasts [19]. (g) Schematic of a heart-on-a-chip supporting valvular endothelial and interstitial cells separated by a porous membrane. (h) Schematic of the co-culturing BBB model with human brain vascular pericytes(HBVPs), HBMECs, and HAs [93]. (i) Layout of a neurovascular unit [94]. (j) Schematic of renal organoid on-chip with a representation of the formation of the vascularized organoid. PSCs: pluripotent stem cells [97]. (a) Reproduced from Ref. [85] with permission of the American Association for the Advancement of Science, ©2012; (b) reproduced from Ref. [86] with permission of the Royal Society of Chemistry, ©2018; (c) reproduced from Ref. [88] with permission of IOP Publishing Limited, ©2019; (d) reproduced from Ref. [27]with permission of the Royal Society of Chemistry, ©2016; (g) reproduced from Ref. [92] with permission of the Royal Society of Chemistry, ©2013.3.1.2. Liver
The liver, considered an organ and the largest gland in the human body, executes several principal functions that regulate the proportion of different indispensable secreted chemicals and components such as cholesterol, triglycerides, and bile [87]. The liver is organized into an almost identical hexagonal lobe, called a lobule, supplied by blood flow from the hepatic arteryand portal vein to the central vein, and bile flow goes through the lobule to the bile duct. More specifically, the lobule can be simplified to a representative unit known as the hepatic acinus. The liver comprises two different cell types: hepatocytes and nonparenchymal cells, including hepatic stellate cells, hepatic sinusoidal ECs, and Kupffer cells.
The construction of in vitro liver models serves as a fascinating application field for bioprinting methods, which allow precise deposition of an undamaged vascularized liver tissue. For instance, a vascularized liver tissue can be achieved using an extrusion-based bioprinting method and opting for an endothelial barrier model. Lee et al. [88] constructed a platform containing an immortalized hepatic cell line (HepaRG) in a decellularized ECM covered by a thin layer of HUVECs (Fig. 6(c)). The device also has an upper channel facing the endothelium barrier (fulfilling the vascularization role) and a lower channel simulating bile flow, making the on-chip device even more accurate. Similarly, in the previously mentioned one-step bioprinted device, Lee and Cho [27] used a bioprinted PCL chip to co-culture hepatocytes in a collagen hydrogel with ECs forming an endothelial barrier (Fig. 6(d)). The vascularized one-step bioprinted liver-on-a-chip was also compared to 2D in vitro models in terms of urea synthesis and albumin secretion to prove the validity and efficiency of the device. In several studies, vascularized livers-on-chips were also realized using microfluidic methods, yet the cells were always exposed to shear stress, which affected their performance.
3.1.3. Skin
The largest organ, the skin, plays a vital role in protecting the body from harmful external factors. Human skin is composed of three layers, starting with the epidermis, which is the outer layer of the skin and is primarily composed of keratinocytes and melanocytes. The second layer is the dermis, which is composed of fibroblasts, macrophages, and mast cells. Finally, the hypodermisis dedicated to fat storage and contains a high percentage of fibroblasts and macrophages. Each layer has specific functions, and all of them permanently interact with the vasculature [89]. Thus, the development of an efficient in vitroskin model is strongly dependent on the development of adequate in vitrovasculature.
Achievement of a reliable vascularized skin-on-a-chip device can be realized by either the angiogenic or endothelial barrier model. Jusoh et al. [90]demonstrated the constructability of the angiogenesis-based vascular skin model by integrating keratinocytes and HUVECs under released pro-inflammatory factors, which later caused angiogenesis of the blood vessels (Fig. 6(e)). Consequently, the microfluidic platform was shown to be useful for testing the effect of chemical irritants such as sodium lauryl sulfate and steartrimonium chloride on the skin. Further research work, led by Mori et al. [91], focused on the importance of the perfusion ability of the vascular channel in an in vitro skin model; the fabrication of a perfusable vascularized model was regarded as a substantial limitation, although necessary. The vasculature was then fabricated by adopting an endothelial barrier model and using a hydrogel-based cell seeding method. The skin-equivalent platform consists of a thin layer of keratinocytes, fibroblast-laden collagen, and a cylindrical endothelial barrier that plays the role of the vascular channel.
Additionally, in a fascinating study, HaCaT cells were co-cultured with ECs and fibroblasts, which were tested with tumor necrosis factor-alpha and caused skin inflammation and edema (Fig. 6(f)) [19]. The three cell layers were cultured based on the cell barrier model and the porous-membrane-based cell seeding method. Overall, vasculature integration provides more efficient drug testing platforms, although bioprinting methods can still be regarded as a potential tool for the co-culture and precise deposition of several cells.
3.1.4. Heart
The heart is a pump that sends blood carrying nutrients, oxygen, and metabolic waste to the rest of the body. It is a continuously active muscular organ with a high need for energy supply and a compact structure. The heart wall comprises several layers, including the endocardium, which is the inner layer in direct contact with the pumped blood inside the heart chambers; the superficial layer is called the pericardium, and most importantly, the myocardium, which is the largest and most rigid layer. The myocardium plays an essential role in generating the aerobic pumping movement; therefore, the oxygen supply must meet the energy requirement in adequate amounts with a well-distributed blood supply. The myocardium is generally targeted when reconstructing the heart because in vitro it has a direct role in the contraction/relaxation phases.
In an early study, Chen et al. [92] constructed a microfluidic platform supporting valvular ECs and valvular interstitial cells embedded in GelMA. The device was separated into two channels by a porous membrane, which collected ECs and formed an endothelial barrier (Fig. 6(g)) [92]. More specifically, vasculogenesis of HUVECs occurred in bioprinted microfibers before the tissue was seeded with neonatal rat cardiomyocytes to form an endothelialized myocardium tissue. A perfusion bioreactor was later added to achieve a vascularized myocardium-on-a-chip model.