1. Introduction
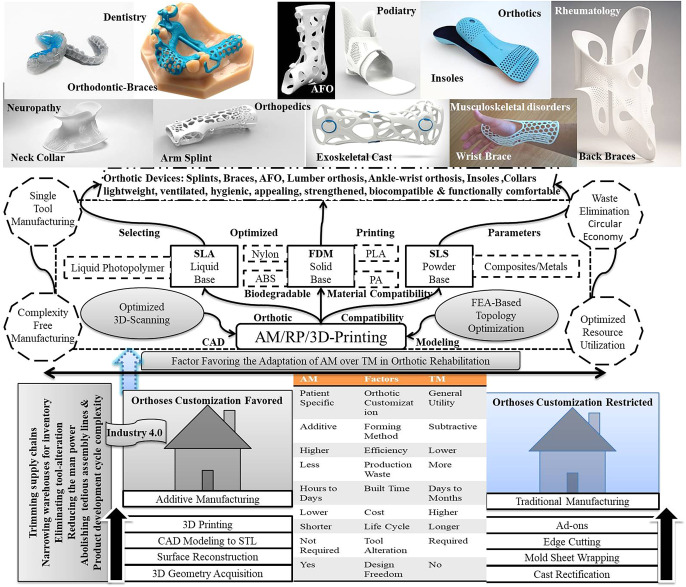
In the past few years, AMT has been universally adopted as a sustainable and efficient platform across all manufacturing sectors (Niaki et al., 2019b). To improve AM performance sustainability, researchers from different specialties are working together to promote the theoretical aspects, technical phases, and application diversity of the process (Ghobadian et al., 2020). The term additive manufacturing or 3D printing is a standard version (ASTM-F2792) of rapid prototyping (RP), which is generally used in many business sectors in the context of developing an immediate product or solution for a given problem or situation under discussion before being getting commercialized (Lee et al., 2016). AM converts a digital data file into a 3D product by additive stacking layer over layer in a streamlined way by reducing the manpower, tool alteration, supply chains, material processing, and product development cycle complexity (Hosseini et al., 2021). Since the beginning (the early 1970s), the AMT has covered a long journey of fundamental and scientific innovations; from simple prototypes to automotive gears, complex jet engine parts, and biomedical implants (Delgado Camacho et al., 2018; Javaid and Haleem, 2018, 2019a). The revolutions' journey started with stereolithography (SLA) in 1984s and is now at a stage where almost thirty different technologies are available for AM; yet, the root process follows the same steps; designing/slicing/fabricating/post-processing to the final product (Jyothish Kumar et al., 2018). The popularity of low-cost portable 3D printers has peaked among individual users, building three-dimensional products by extruding plastic filament wire rolls and depositing the molten layers with rapid cooling (Ngo et al., 2018). The more affluent 3D printers are bigger and capable of producing large build volumes like structural parts (i.e., houses) through binding multi-materials using laser-based and other advanced, accurate & proficient technologies (Bandyopadhyay and Heer, 2018). The availability of reliable, economical, portable, user-friendly, fast, and accurate 3D printers has increased AMT's market over trillions of dollars and the industry is forging ahead from single user interface to mass production platform (Kleer and Piller, 2019). AM's application diversity is now presenting a new picture of sustainable business transformation in the global health market by taking the prodigious lead over traditional manufacturing (TM), as shown in Fig. 1 (Irfan Ul Haq et al., 2020). A broader scenario rooting from the sustainable adoption of 3D printing for customized rehabilitation has been expanded to the technical diversity of structural optimization (as shown in Fig. 1), integrating environmental safety with product compatibility.
 Fig. 1. Rise of additive manufacturing in orthotic rehabilitation.
Fig. 1. Rise of additive manufacturing in orthotic rehabilitation.When the demand for a specific product arises in bulk, only then an industry plans to reschedule the entire product development cycle, including product designing studios, supply chains, processing & assembly lines, which involves both economic and aesthetic issues (Kumar et al., 2016). It is impossible for patients to instantly get a medical aid like a prosthetic or splint as per their anatomical assets for rehabilitation from such a mass-oriented industry. Here AM plays the role of a life savior, bypasses all the manufacturing & distributary hurdles through on-spot fabrication of patient-specific customized utility, and provides a sustainable solution (Hosseini et al., 2021). It eliminates the requirement of large warehouses for inventory, trims the long supply chains for material processing, abolishes tedious assembly lines by single-piece product fabrication, and enables on-demand on spot production as per the need, which adds to the sustainable flexibility of the process (Bhasin et al., 2021). Simultaneously it provides better economic products, where it is more complicated to produce such complex geometries by traditional units; the complexity-free manufacturing attribute of AM cost-effectively reflects the same by minimizing the workforce and material consumption (Pereira et al., 2019). Also, there is a considerable impact of 3D printed (3DP) orthotics on the patient's sustainable rehabilitation because the AMT enables to produce light weight multi-colored best fit prosthesis as per user sensitivity & limb-anatomy, which in result has a great impression on the physical and psychological healing of the patient (Soares et al., 2021). AM provides an effective & economical solution over TM when an urgent demand arises for an orthotic device with user-specific, complex customized geometries (Choo et al., 2020).
An Orthotic device, i.e., splint/brace/orthosis, provides functional assistance to the limb's musculoskeletal system by supportive weight balancing to the deformity for motion assistance/restriction in the form of a protective cast to cure dysfunctions or injuries (Soares et al., 2021). Depending upon the affected joints in the body, they can be classified into three segments; lower limb orthoses (ankle-foot orthoses/AFOs), spinal orthoses (lumbar orthoses), and upper limb orthoses (hand wrist orthoses) (Barrios-Muriel et al., 2020). Orthotic devices have existence in human society from the early ages for giving similar therapy; the structures & materials get updated with the technical innovations from wooden/leather supports to 3DP customized bioplastic splints (Shahar et al., 2019). The traditional orthosis methods are inefficient, time-consuming, unpredictable for repeatability, and deliver inflexible heavyweight casts (Alqahtani et al., 2020). The appliance process also involves the manual corrections for getting the required shape and a highly skilled orthotist, which creates an irritating and painful situation both for the patient and the operator (Wang et al., 2020). Such orthosis delivers undesired stresses even over the healthy muscles & ligaments rather than localized support over the concentration point (Guida et al., 2019). In such cases, AM successfully addresses TM's aforesaid limitations and provides an economical, customized, flexible, topologically optimized orthotic device, directly from the 3D scans, as per the patient's limb anatomy (Thomann and de Carvalho, 2019).
With the advances in design engineering, structural optimization has enabled designers to develop sustainable and lightweight products for better performance (Dillard, 2010). The constraints involved in TM bounds the designers to think about the feasibility of topology-optimized products (Liu et al., 2020). In the counterpart of the arena, the potential capability of AM promotes the developers to work on TO of the structure for reducing the mass & material while maintaining/enhancing the functional reliability of the final product (Geoffroy et al., 2018). Yet, the TO methods have been efficiently deployed, tested and evidenced for redesigning the structural mechanics in various engineering fields, but there is still an application gap between the assistive enactment of TO with healthcare and orthopedic rehabilitation. One of the major reason for the inefficient immersion of TO in orthotics includes; lack of the available literature accounting the data analysis results over functional outcomes and biomechanical performances of topologically optimized orthotic devices. Sometimes, practitioners face trouble defining the set of TO constraints for anatomical structures, especially in the dynamic loading conditions, where the limited mathematical equations specifically demanded for responsive load computation make the situation more complicated. Also, one of the critical challenges is the lack of an integrative AM framework that can optimize the design's topology, subsequently interpret the optimization results into the printable STL format and successively define the optimum printing parameters to have digital control over the AM process for availing the patient's specific orthotic devices.
The strategic involvement of AM in the medical industry with topologically optimized products can ensure the performance sustainability over its rivals in a competitive global environment by meeting economic, environmental, and aesthetic issues (Niaki et al., 2019b; Pearce et al., 2019). In this paper, a systematic approach has been discussed to understand the role of AMT in sustainable rehabilitation (second section), the complete process of realizing orthotic devices using AM along with the recent advances in 3DP orthotics (third section), and the role of topologically optimized orthotic devices in rehabilitation engineering market has been discussed with a novel proposal of systematic multidisciplinary AM framework for orthotics (fourth section). This paper can provide future guidance to the researchers for further advances in orthotic science and offer a dominant intimation to the manufacturers to lead within the healthcare and rehabilitation industry.
2. Determinants favoring the adoption of AM in healthcare over TM
The vast opportunity criterion of AM is now getting the attention of academic researchers, professional designers, manufacturing practitioners, economists, and environmental activists for adopting the technology as a sustainable alternative to TM in healthcare (Chatwani et al., 2021). AM can accelerate the product development cycle and make the approach more cost-effective by reducing the operational cost in manufacturing with lesser consumption of resources. The medical industry is a suitable segment where the potential of AM can be used for the sustainable rehabilitation of humankind (Ashima et al., 2021). The applications of AM in the medical healthcare industry are growing day by day with patents and innovations, which can be classified into six major groups; tissue & organs, prosthetic & orthotics, anatomical models & surgical equipment, drugs & medicine, body implants, and dentistry (Li et al., 2020; Maniruzzaman, 2019).
Before implementing any manufacturing strategy, it is necessary to understand its primary professional benefits at the initial, intermediate, and final stages. In this section, some of the potential benefits of AM have been reviewed to answer the question; why AM is getting more attention from the manufacturers over TM in the survival race for ensuring a bright future in the competitive, sustainable healthcare society, as shown in Fig. 2. A sustainable society ensures the prosperous development of humanity and promotes activities that offer energy conservation, resource reutilization and socio-economic equity for employees, manufacturers, and consumers (Giannetti et al., 2021; Panizzut et al., 2021).
 Fig. 2. Significant characteristics of AM and potential benefits over TM.
Fig. 2. Significant characteristics of AM and potential benefits over TM.2.1. Constraints-free geometrical realization offering flexible customization
In AM, digital design data files are treated as inputs, as there are no such constraints over a designer's creativity; the product complexity isn't considered a virtue, providing a strong hand to AM over TM. AMT facilitates the fabrication of any complex geometry directly from digital data and maintains most of the shape and structural features in the product. A passive-dynamic AFO was fabricated using selective laser sintering (SLS) to replicate the shape and functional features of traditionally made carbon-fiber AFO, showing the substantial response for mechanical damping and energy dissipation in the walking application (M.C. et al., 2008). The 3DP skins with the replicated structural properties are frequently used as an alternative to animal skin, for testing the various chemical, cosmetics and pharmaceutical ointments (Trenfield et al., 2019). When dealing with anatomical structures, it is complex to draw body curvatures precisely in computer-aided design (CAD) models; in such cases 3D scanners accurately conclude the task of geometrical acquisition (Javaid et al., 2020). Especially when dealing with medical equipment like orthopedic devices, a portable 3D scanner makes the task much easier, by on-spot scanning of the body part and enhancing AM performance sustainability for custom-fit orthoses (Javaid and Haleem, 2018).
The additional consequences of design freedom can be realized as weight reduction and mass cutting by optimizing the topology of the product, which ensures the evasion of waste, cost reduction, and energy savings in production phase (Liu et al., 2018). AM based on biomimetic design, especially in the medical domain, can enhance the performance of scaffolds, implants and orthotic devices by weight reduction up to a considerable level and minimum material usage (Muthu, Subramanian Senthilkannan; Savalani, 2019). The AMT has been adopted for commercial production of AFOs, as per the clinical recommendations for treating rheumatoid arthritis and clubfoot defect (Wojciechowski et al., 2017; Pallari et al., 2010). Product design diversity offered by AMT promotes the designers to replicate componential products into a one-piece entity, which endorses the idea of assembly-free production (Oh et al., 2018). It eliminates the component manufacturing cost, assembly cost, and assembling errors, making the product more precise and economical (Sauerwein et al., 2019). Freedom to design in AM boosts the user's innovative aggression to improve product quality, durability, and functionality by providing better suggestions in the market over the available traditional products as a micro-manufacturer. SLS-based glove fit foot insoles for providing biomechanical comfort assistance to the runners were tested for three months and found to be more comfortable than the commercially available products in the market with better injury prevention (Salles and Gy, 2013).
2.2. Sustainable single tool manufacturing
AMT works on the practicality of fabricating the final product directly from the design data without complementary tools and equipment (Srivatsan and Sudarshan, 2015). A 3D printer independently fabricates the final product by additive deposition of thin layers without changing tools or altering the molds as required in TM (Jiang, 2020). In TM, a product is developed by the controlled removal of excess material from the raw bunch, a subtractive manufacturing approach that progressively requires unique jigs, fixtures, and tools (Watson and Taminger, 2018). In AM, the printing device itself concludes the fabrication task; opposite to TM it works on the additive principle of manufacturing, eliminating the fixed cost, tool changeover cost, and time (Baumers et al., 2016; Thomas and Gilbert, 2014). The AM offers a more competitive platform for enhancing the circular economy in small production runs, especially in dealing with standardized orthoses, prosthetics and implants (Kumar et al., 2021; Ramola et al., 2019). The AMT is so dynamic that the same 3D printer that has been used for producing orthotic devices can also be used for fabricating implants, anatomical models, braces, surgical equipment, simply by altering the designs and materials, without any material processing add-ons (Culmone et al., 2019). AM enables the user to fabricate different products as per application diversity, in a fully customized manner, from single equipment, without substitutes. It also refurbishes the mass economy into a single product economy by favoring on demand-on-spot production, which diminishes the inventory budget (Thomas, 2016). Even the multi-material splints can be developed using a single machine, enhancing the product's functional performance in terms of stiffness and providing psychological healing assistance with its appealing looks (Venumbaka et al., 2020). Since the TO-based single tool AM can mix the multiple salts, it can deliver distinct hybrid tablets in the future that can replace multi-medicine doses and make the prescribed dosage routine leisure. Also, the tablets' optimized shape and surface area can accelerate their dissolving rate, reducing the reaction time and providing instant relief to the patient.
2.3. Sustainable utilization of resources
AM is referred to as direct design manufacturing because it simply converts any design file into its realistic 3D contour, ensuring the optimized utilization of resources with minimum consumption of man, material, and money (Sanchez et al., 2020). In the metal sintering-based fabrication, the AM ensures almost 95–98% reutilization of raw material, which is not got sintered in earlier production, is reutilized for impending one (Hitzler et al., 2018). The AM process doesn't pass through the intermediate stages of the production line as implemented in TM, saving a lot of time, energy, and workforce and reducing supply chain complexity (Niaki et al., 2019a). In emergency cases, rather than refereeing the patients to specialized labs for intraoral images, small portable 3D scanners can provide immediate scans and saves a lot of time by providing digital dentistry service (Javaid and Haleem, 2019a). The AM approach can handle the environmental issues of a manufacturing firm in a far better way by implementing a process parameter optimization approach (Böckin and Tillman, 2019). Specifically, the energy efficiency can be improved significantly by TO of the design for a given production volume over-optimized input variables. (Hopkins et al., 2021) revealed some valuable semi-empirical equation-based prediction methods (max. error ±3%) to measure and minimize the energy consumption in the low-cost desktop 3D printers by suitably selecting optimum build parameters. (Barros et al., 2017) conducted life cycle assessmentexperiments to evidentially understand the environmental impacts of AM by comparing 3DP orthotic insole with a classical handmade insole. The study recommended the adaptation of AM as a business opportunity by the professional due to its considerable manufacturing impacts on the ecosystem, health, climate, and resources. Also, the social implications of AM can't be ignored; it connects the developing society with modern technology and provides fortuity to join the emerging global market as a platform to present their ingeniously designed products (Matos and Jacinto, 2019; Steenhuis and Pretorius, 2017). It promotes a user-friendly healthy workspace in an industry and evades physically exhaustive and hazardous working culture as in TM (Huang et al., 2013). The capability of the process to deliver patient's specific customized equipment loaded with professionally recommended attributes along with individual's taste, supports the healing psychology and aesthetic guts in the user for sustainable rehabilitation (Blaya et al., 2018). Fancy transparent 3DP orthodontic devices instead of lewd metallic braces, are frequently used to straighten teeth with better comfort and outlooks (Lee Ventola, 2014).
These significant credentials give industrialists a better choice for adapting AM rather than TM for numerous sustainable benefits with economic, environmental, social, individual and global assistance (Agrawal and Vinodh, 2019). Altogether these favorable potential traits ensure an optimistic future of the technology, particularly in the medical industry, it demands the researchers to pay more attention to promote functional outcomes on a global platform presenting qualitative & quantitative comparison matrices in parallel with TM (Ghomi et al., 2020). Some of the technical issues must be addressed profoundly at the R&D level, like improving build size & printing speed to make the process faster and reliable (Prabhu et al., 2020). A team of worldwide researchers must be executed to develop systemic multidisciplinary software that can digitally control the entire framework; design evaluation to AM, and then to the functional assessment of the products to project the AMT for mass production.
3. Material and methods involved in orthotic realization by AM
The conventional method for manufacturing the orthotic products usually involves plaster casting, which is less expensive, the user requirement for customized body fit is not fulfilled up to that extent as overlaid with AM (Fitzpatrick and Gibson, 2019). In the case of any medical emergency related to musculoskeletal injury or deficiency, the patient has to consult with the orthopedist and then meet with orthotist for anthropometric measurements (Graham et al., 2020). Traditionally the process starts with initial wrapping of stocking, cotton wraps, and plaster bandages over the affected limb for obtaining a mold cast. Successively, manual cast molding is done with repetitive plaster pouring to get a positive mold with uniform fitness. Afterward, a heated-vacuum casing of polyethylene/polypropylene thermoplastic sheet is done over positive mold and left to cool down for the desired shape. Sometimes post-processing operations are performed to add supportive components or trim the undesired ones, as per the stresses over the affected area (Fitzpatrick and Gibson, 2019). The existing process is tedious as it involves long plaster settling time, high clinical cost, wastage of raw material, manual pressure approximation to avoid overfitting & loose-fitting and repetitive clinical visits to ensure amenity and functionality of the orthosis (Guida et al., 2019). Also, in TM the quality of the product is significantly dependent on the practitioner's experience and skills; the repeatability is always an issue. AM is a highly automated process based on the industry 4.0 concept, which ensures limited human involvement only in the early designing phases, and is capable of fabricating custom fit orthosis in a shorter execution time with maximum accuracy and minimum wastage (Mehrpouya et al., 2019). In this section, sequential stages involved in AM of an orthosis are explained in detail with their working principles, convenient applications and possible alternatives, along with its brief contribution in recent years for sustainable orthotic rehabilitation, as shown in Table 1. The fundamental procedure for availing the anatomical products includes geometry acquisition, surface reconstruction & CAD modeling, design conversion into a standard printable format, and printing the design to avail the custom fit orthosis. It is broadly classified into two major sub-groups one is geometrical design modeling and another is 3D printing.
Table 1. Recent advances in 3DP orthotics and implications over sustainable rehabilitation.
|
AM Method |
Data Acquisition Pathway |
Material Used |
Applied Orthosis /Body Part |
Objectives | Sustainable Rehabilitation Outcomes/Results | Study | Year |
|---|---|---|---|---|---|---|---|
|
3D Printing: Fused Deposition Modeling (FDM) |
3D Scanner (Structure sensor based) | Thermoplastic elastomer | Thumb orthosis (upper-limb) | To check the feasibility of getting a short limb orthosis from the optimized reverse engineering of a parametric hand model and perform functionality evaluations of the 3D printed (3DP) orthosis |
Enhanced movement flexibility in texting, writing, playing computer games and high score in Quebec evaluation for user satisfaction (4.9) Reduction in cost and time for model creation |
Chu et al. (2020) | 2020 |
| 3D Printing (specification not provided) | 3D Optical scanner | Light-activated resin | Wrist-hand orthosis (upper-limb) | To compare the performance of 3DP wrist-hand orthosis with low-temperature thermoplastic plate orthosis on wrist flexor spasticity in chronic stroke patients | 3D printed wrist hand orthosis performed more satisfactorily in reducing swelling and spasticity. Also, significant support in motor functions and extension of passive-range | Zheng et al. (2020) | 2020 |
| 3D Printing (specification not provided) | 3D Surface scanner | Nylon | Foot orthosis (lower-limb) | To extract the conclusive evidence for dealing with foot pronation by comparing the running biomechanics in three different running conditions: along with traditional plaster molded (TPM) foot orthosis, 3DP foot orthosis, and no-orthosis control condition (CON) | TPM & 3DP orthosis resulted better perceived comfort than CON (heel cushioning: 6.9/6.1 & medial-lateral control: 6.5/6.2). Yet, no considerable statistical differences between TPM and 3DP orthosis parameters | Mo et al. (2019) | 2019 |
|
3D Printing: Fused Deposition Modeling (FDM) |
CAD/Footscan® 3D gait analysis system | Polyethylene acetate | 3DP AFO: Insoles (lower-limb) | To investigate the effect of customized 3DP AFO on plantar biomechanics and the level of comfort offered in plantar fasciitis in comparison with traditionally pre-fabricated one |
3DP-AFOs have significant potential to reduce damage associated with plantar lesions and are useful in treating plantar fasciitis. Visual analog scale(pain):3DP/Prefabricated after 8 week = 3.12 ± 0.51/5.25 ± 1.22 |
Xu et al. (2019a) | 2019 |
|
3D Printing: Fused Deposition Modeling (FDM) |
3D Laser scanner |
Modified thermoplastic: Acrylonitrile butadiene styrene (ABS) |
Wrist-hand orthosis (upper-limb) | To replace the plaster cast with 3DP orthosis and check the treatment feasibility in pediatric nondisplaced metaphyseal distal fractures | High overall patient satisfaction (4/5) Enhanced functionality and reduced pain (patient-rated wrist evaluation: 4.3 ± 4.00 & 4.30 ± 5.60). | Guida et al. (2019) | 2019 |
|
3D Printing: Fused filament fabrication (FFF) |
3D Scanner |
Thermoplastic Polyurethane and polylactic acid |
Wrist-hand orthosis (upper-limb) | To assist the hand functionality in daily routine activities like writing, typing and eating for the individual suffering from hemiparesis |
Quebec evaluation (writing/eating/typing: 31/35/38) Jebsen test (writing/eating/typing:43.2/12.3/22.3) |
Lee et al. (2019) | 2019 |
|
3D Printing: Fused Deposition Modeling (FDM) |
CAD/Footscan® 7 gait 2nd generation system | Polyethylene acetate | 3DP Insole | To investigate the functional performance of 3DP customized insoles to assist comfort and plantar pressure for flatfoot symptomatic patients | Reduction in mid-foot peak pressure. Higher visual analog comfort score, measured by pain scale (after 8 weeks: 3DP/prefabricated = 2.42 ± 0.13/5.92 ± 1.19) | Xu et al. (2019b) | 2019 |
|
3D Printing: Fused Deposition Modeling |
3D Scanner | Polyethylene acetate | 3DP Insoles (lower-limb) | To test the pressure distribution performance of arch lift based 3DP heel support insoles in maintaining foot functions through plantar parameters measurements | Arch lift-based 3DP insole/3DP insole/traditionally available insole (A/B/C): reduction in under heel peak pressure (170/200/260 in kPa). Enhanced (A) movement stability and biomechanical performance | Jin et al. (2019) | 2019 |
|
3D Printing: Fused filament fabrication (FFF) |
CAD Modeling |
Thermoplastic PLA |
Wrist Driven Orthosis (WDO) (upper-limb) |
To design and collect the user (N = 3) feedback for enhancing the functions, accessibility and customizability of 3DP WDO for individuals with spinal cord injury |
Jebsen hand function test: Increase in grasp strength (13–122%). Enabling to perform pinching grasp and small object tasks. Average score by users: 6.8/7.7/7.7 |
Portnova et al. (2018) | 2018 |
|
3D Printing: Fused filament fabrication (FFF) |
3D Scanner/CAD | Thermoplastic polyurethane | Wrist orthosis (upper-limb) | To compare the performance of 3DP wrist orthosis with cock-up splint for patients with wrist pain | 3DP wrist orthosis gained a high satisfaction score in orthotics and prosthetics user survey (P = 0.036) | Kim et al. (2018) | 2018 |
|
3D Printing: Fused Deposition Modeling (FDM) & Streolithography (SLA) |
3D Optical scanner |
PLA ABS Photosensitive resin |
Hand fingerboard (upper limb) | To elaborate on the clinical efficiency of 3DP customized fingerboard in the preventive treatment of finger spasms for cerebral stroke patients | Enhanced comfort with no skin allergy and worsened pain (1.69 ± 1.03). Assistive tension (1.73 ± 0.70) and bending resistance with improvised hand functions, motion range (3.23 ± 0.83) and grip strength (0.032 ± 0.067) | Wang et al. (2018) | 2018 |
|
3D Printing: Selective Laser Sintering (SLS) |
MRI & CT | Polypropylene and polyamide | Wrist-hand orthosis (upper-limb) | To check the clinical outcomes of 3DP cast in terms of patient satisfaction and clinical efficacy during a six-week follow-up for the treatment of distal-radius fracture |
Questionnaire-based (In terms of pain, blood circulation, stability and pressure): User satisfaction (11.5/15) & clinical efficacy (9.8/12) |
Chen et al. (2017) | 2017 |
|
3D Printing: Fused Deposition Modeling (FDM) |
3D Scanner | Polyethylene acetate | 3DP insole (lower-limb) | To compare the shape based insoles with virtually optimized milled and 3DP insoles to compare their pressure offloading performances over planter tissues to avoid risk of ulceration | A considerable reduction in peak pressure by a mean of 40.5 kPa for 3DP and 41.3 kPa for milled compared to shape based insoles. | Telfer et al. (2017) | 2017 |
|
3D Printing: Fused filament fabrication (FFF) |
3D Scanner | Thermoplastic polyurethane | AFO (lower-limb) | To design, fabricate and record clinical gait performance of 3DP AFO for foot drop patient by the sequential passage through mechanical stress test and durability test | 3DP AFO/Conventional AFO/No AFO: Gait speed in cm/s (56.5/56.5/42.2), step width in cm (15.9/17.1/17.9), user satisfaction Quebec evaluation (4.5/4.1) | Cha et al. (2017) | 2017 |
|
3D Printing: Selective Laser Sintering (SLS), Fused Deposition Modeling (FDM) |
3D Scanner, CAD, CREO Parametric | Nylon (SLS), PLA (FDM), carbon-filled PETG (FDM) | AFO (lower-limb) | To test and validate the efficacy of three different 3DP custom fit AFOs and automate the orthotic design and manufacturing processes | Nylon was suggested for fabricating single-piece AFOs (no fracture up to 5% of strain) The values of yield stress for PETG and PLA samples were close in range (97 MPa & 88 MPa) and the PLA was suggested for higher fracture strain and low cost of printing. | Walbran et al. (2016) | 2016 |
|
3D Printing: Polyjet printing (inner structure) & injection molding (outer cover) |
3D Laser scanner | ABS plastic material (3DP) & polycarbonate material (injection molding) | Wrist orthosis (upper-limb) | To reduce the manufacturing time and cost for availing customized wrist orthosis by adopting a hybrid fabrication approach combining the potential benefits of 3DP and traditional injection molding | 3DP orthosis offers enhanced ventilation, strength improvisation and weight reduction. Significantly the time cost for orthotic manufacturing was estimated 1/3rd of that of the other methods | Kim and Jeong (2015) | 2015 |
|
3D Printing: Fused Deposition Modeling (FDM) |
3D Scanner | Acrylonitrile butadiene styrene (ABS) filament | Custom foot orthosis (lower-limb) | To interpret the opportunity of low-cost 3D scanning & printing for availing customized 3DP foot orthoses and compare its gait kinematic outputs with traditional plaster cast orthoses | Increase in arch height index (AHI in mm) with 3DP orthotics compared to shod condition (3DP/shod/plaster cast: 21.5 ± 0.96/21.2 ± 0.83/22.0 ± 0.84) | Dombroski et al. (2014) | 2014 |
|
3D Printing: Fused Deposition Modeling (FDM) |
3D Scanner | Polylactide | 3DP customized foot orthosis (lower-limb) | To investigate varying dose effect of 3DP foot orthosis on plantar pressure and electromyographic (EMG) activity in the asymptomatic and symptomatic pronated foot types | 3DP customized foot orthoses have a significant linear dose-response effect on plantar pressure variables at lateral rearfoot (mean P = 0.001), midfoot (peak/mean: P˂0.001) and forefoot (peak/mean: P˂0.001) | Telfer et al. (2013) | 2013 |
|
3D Printing: Selective Laser Sintering (SLS) |
3D Scanner & CAD | PA2200 Nylon-12 powder | Foot orthosis (FO) and AFO (lower-limb) | To evaluate the compatibility of 3DP FO for releasing pressure at metatarsal heads & 3DP AFO for attaining adjustable stiffness in sagittal plane, under various biomechanical modes of action |
3DP FO with adjustable elements reduced the pressure under targeted metatarsal heads (1st: 21.9 kPa, 2nd: 22.9 kPa & 3rd: 12 kPa). 3DP AFO with varying stiffness, offered favorable support to ankle kinematics (reduction in peak ankle internal plantar flexion moment than shod (p˂0.001)) |
Telfer et al. (2012) | 2012 |
|
3D Printing: Selective Laser Sintering (SLS) |
CAD Modeling | DuraForm EX natural plastic (3D Systems) | PD-AFOs (lower-limb) | To develop a novel design customization and manufacturing framework for 3DP PD-AFOs and verify the dimensional accuracy of the orthotics | For the four half-scale orthoses, dimensional discrepancies were within a tolerance of 2 mm and for mean foot plate/strut/cuff/overall orthosis discrepancies were 0.31 ± 0.28/0.34 ± 0.08/0.52 ± 0.39/0.29 ± 0.23 mm | Schrank and Stanhope (2011) | 2011 |
|
3D Printing: Selective Laser Sintering (SLS), Stereolithography apparatus (SLA) |
CAD Modeling |
DuraForm® PA (3D Systems 2009a), Polyurethane (PU) foam |
Pedorthoses (lower-limb) | To transform the customized CAD models into 3DP functional pedorthoses and test the validity for improvement in mobility for clubfoot correction | Among the five 3DP pedorthoses fabricated successfully (N = 4 patients), only one soft insert and hard shell needed replacement during first seven month of use and found accurate-fit, durable, adjustable and effective in clubfoot correction | Cook et al. (2010) | 2010 |
3.1. 3D anatomical morphology/geometry acquisition practices
Application diversity in AM has extended the domain of the data acquisition techniques, starting from professionally designed geometries in CAD to direct limb morphology acquisition using CT scans and 3D scanners (Barrios-Muriel et al., 2020; Javaid and Haleem, 2018). Depending upon the approach implemented for geometry acquisition, the collected data can be characterized as volumetric elements (voxels) designated with 3D colored coordinates or in the form of point cloud data, representing different anatomical points. The AM process of orthotic fabrication is not tied with any standardized procedure for anatomical morphology acquisition; some of the professionally designated techniques have been discussed in this section.
3.1.1. CT-MIMICS-CAD sequentially integrated approach
Computed tomography (CT) is a well-known computer-assisted medical imaging technique for getting internal anatomical views of the body without dissection through digitally controlled multi-angular X-ray measurements (Thompson et al., 2017). Yet CT is a professionally adopted technique for internal disease diagnostic and for planning the relevant surgery, therapy or biopsy, still high-resolution CT scans can also be used for orthotic design by following an ordinary procedure (Choi et al., 2019). CT scan of the concerned body part provides image slices in DICOM format, further utilized by MIMICS software for the 3D volumetric reconstruction based on the grey intensity concept (Mohite et al., 2020). In MIMICS, the imported DICOM slices are arranged at an adequate slice distance, followed by thresholding and segmentation analyses to remove undesired tissues & bones and for filling the voids in the 3D model (Pardo et al., 2020). The model file in standard STL format is then imported into CAD software to obtain a printable standard 3D solid model by adding supportive structures through the various designing, meshing & Boolean operations (Lal and Patralekh, 2018). An integrative approach using CT, MIMICS and CAD was exercised to develop a reliable custom-fit foot orthosis design, comparatively in a lesser time for the rehabilitation of leprosy patients in terms of stability and comfort (Paul, 2012). In integration with AM, CT data can be utilized effectively to fabricate functional gradient-based insole structures with large contact areas for customized stress distribution and peak pressure reduction to lower the risk of diabetic foot (Tang et al., 2019). The functional auricular products fabricated by fused deposition modeling (FDM) based AM and CT scans have exceptional mechanical resistance with negligible dimensional error (0.1–3%) and that's why preferred over traditional one (Artioli et al., 2019). This integrated designing approach have its potential modelling utilities in multiple aspects as in orthotics, prosthetics and for implants as well, the radiation downsides are always creates insecurity over long anatomical scanning intervals. The CT provides sporadic resolution between tissue images still the blurred boundary can't be avoided in the cases when several densities share similar pixels causing partial pixel effect.
3.1.2. 3D scanning with reverse engineering
The images captured by CT and MRI are promptly used for reconstructing surgical practice-based structural models for the internal organs, bones, and tumors, it provides a proficient opportunity for mutual execution of surgical implants and orthoprosthetic devices (Fernandez et al., 2020; Tzavellas et al., 2020). Especially when the target is to design the customized 3D models for the external body parts like orthotics and prosthetics, the 3D scanning approach delivers a better elucidation that is more convenient, economical and contented (Javaid et al., 2020; Javaid and Haleem, 2019b). 3D scanners basically work on a light projection model to collect points cloud mesh containing informative three-dimensional positions of surface points in 3D space to precisely retrieve the entity's surface using dedicated software (Shih et al., 2017). The mesh data transformation using specialized software avails parametric 3D model in STL format, feasible to be 3DP directly, or retrieved in CAD if additional features are to be superimposed. There is a wide choice for 3D scanners offered in the market some of them are laser-based, some are loaded with projected cameras and some are mutually equipped with both laser projectors and tracking cameras (Javaid et al., 2020; Shah and Luximon, 2017). 3D scanning is vastly preferred for orthoses fabrication in clinical and academic trials for functional and experimental purposes because it offers less recording time, error-free precise topography, and on spot instant scans for immediate treatment (Haleem and Javaid, 2019). The advantage of 3D scanning raises the concept of reverse engineering for digitizing the 3D anatomical scans as per the expert's interest using appropriate modeling software to develop a simulated orthosis model before moving towards the AM of the final product (Baronio et al., 2016a). The passive stereo photogrammetry based 4D image capturing techniques can be positively integrated with reverse engineering practices for clinical observations and AM of FDM-based customized wrist orthosis (Palousek et al., 2014). An integrated designing and fabrication approach was proposed for the economical production of 3DP AFOs to replace traditionally made orthoses followed by 3D scanning, CAD modeling, finite element analysis (FEA), and theory of composites (Banga et al., 2018). A systematic workflow embedded with smart algorithms was developed for AM of bespoke device from validated 3D scanned data, by effective distribution and cutting of padding material in the orthosis geometry and to rehabilitate cervical instability of the neck (Hale et al., 2020a). The 3D scanning approach offers affordable efficient hardware and accessible user friendly software for the external topography measurements, still sometime it is difficult to capture thin and long extruded parts like hairs, finger gap and the intricate wrinkles, folds and curvatures, in a single scanning turn and that's why sometime complete geometry is captured in multiple scanning passes. Still, when the task is to deliver immediate functional supports for musculoskeletal injuries, the 3D scanning embedded with reverse engineering efficiently assists the AM of upper & lower limb orthoses because it is an affordable, portable and accessible data acquisition approach that doesn't demand specialized labs and highly trained operatives for handling (Anggoro et al., 2018; Volonghi et al., 2018a).
In some cases, to acquire standard kinematic protocols, the dynamic topographic measurements are taken using marker-based optical motion capture systems to enhance the orthotic rehabilitation under dynamic loading conditions (Mo et al., 2019).
3.2. Fabrication technologies frequently adopted in AM of orthoses
The combination of 3D scanning, reverse engineering and AM is a stoutly emerging approach that is receiving further attention over various traditional casting practices in the field of medicine and orthotics (Baronio et al., 2016b). A standard AM approach tracks a series of sequential phases for fabricating customized orthotic devices; anatomical topography acquisition via 3D scanning, meshing/editing/modeling in a design software (ex; CAD/CREO) to get standard (STL format) design file of the parametric model, slicing the digital model and setting printing parameters in a design translation software (ex; CURA/SLIC3R) and translating the printable design file to a digitally controlled 3D printer for additive printing of the sliced layers to obtain a functional 3D model of the orthotic device. Clinicians widely prefer the AMT to avail the patient's specific customized orthotic devices over the standard plaster casting for better user comfort and shorter delivery time (Hale et al., 2020b; Portnoy et al., 2020). The technique is also preferred because it offers design creativity, design flexibility, customized designs with functional & supportive elements, précised fitting with accuracy, lesser designing and printing time and overall sustainable rehabilitation feedback at the end-user level (Chae et al., 2020; Chu et al., 2020).
AM is a well-known fabrication technique that converts a standard digital format of design (STL format) into its realistic 3D model by additive deposition of thin layers (up to 0.1 μm), tallying exact amount of material that is needed to complete the job without wasting the material, money, manpower and machine energy (Gibson et al., 2021). The AMT can be classified into various segments depending upon the mechanism of fabrication approach (vat polymerization, material extrusion, power bed fusion, sheet lamination, binder jetting, material jetting and direct energy deposition) and the nature of the material being used (powder, wire, filament, liquids, gels, concrete, aerosols and cells), the basic idea that is controlled digital fusion of raw material remains same in all the ways (Bandyopadhyay and Bose, 2019; L. J. Kumar et al., 2018). Among the variety of resourceful methodologies, a few of them are sustainably adopted for fabricating orthotic devices, which are discussed briefly in this section.
3.2.1. Material extrusion-based fused deposition modeling (FDM)
In the FDM process, also known as fused filament fabrication (FFF), material filament is fed by extruder into the print head, which is equipped with heating elements and printing nozzle, it deposits the 2D layers (0.1–0.5 mm thick) of semi-molten material one by one to build a 3D product (Mwema and Akinlabi, 2020). Some of the FDM printers are equipped with dual print heads, one for building the main structure and the other one for a temporary support structure for the overhanging parts (Chua and Leong, 2014). The most common materials used to make FDM parts include various thermoplastic polymers like; nylon, acrylonitrile butadiene styrene (ABS) and polycarbonates (PC) which are frequently adopted for producing both testing prototypes and production products (Penumakala et al., 2020). FDM can fabricate parts 85% as strong as molded products, with lesser consumption of material over varying infill densities (10% for fitting prototypes, 20% for building tradeoffs and 80–100% for heavily strengthened products) (Mwema and Akinlabi, 2020). (Chadha et al., 2019; Deshwal et al., 2020) investigated the effect of various printing parameters on the FDM products and found that the mechanical behavior of the fabricated parts especially the strength, can be enhanced at optimized printing speed, infill densities and build temperature. The key factors behind its adoption for orthotic devices include readily accessible cheaper 3D printers, easily available economic raw materials, ease of equipment & material handling and lighter & strengthen product delivery (Ambu et al., 2020; Barrios-Muriel et al., 2020). Most of the academic, experimental, industrial and clinical 3D printers come under this category, making it a globally adopted technology for AM of orthotic devices. (Baronio et al., 2016b) adopted low-cost FDM printing technology and 3D scanning approach to provide an economical solution for fabricating customized upper limb orthoses. (Ambu et al., 2020) suggested FDM as a far better option for producing customized neck orthosis than traditionally available medical devices, and used a hybrid composite material to fabricate lightweight, hygienic, ventilated and breathable cervical orthosis constituting honeycomb/elliptical geometrical patterns. (Redaelli et al., 2020) proposed an innovative production approach to fabricate scoliosis braces by FDM printing and checked their morphological properties against classic thermoformed braces, and recorded better stiffness characteristics.
3.2.2. Powder-bed fusion-based selective laser sintering (SLS)
SLS based AM is profoundly used for fabricating metallic (Steel, Cobalt, Inconel and Aluminum) as well as non-metallic (ceramics, glass, thermoplastics; polyamide, ABS and PC)) products for higher strength and accuracy (Schmid et al., 2014). SLS works on the fused powder sintering concept, where powdered material is heated near to its melting temperature and selectively fused with an intense CO2 laser beam to fabricate first layer (0.02–0.08 mm) of required geometry (Davim, 2020). The process is repeated by wiping a fresh powder layer over the powder bed for sintering the next layer, with successive downward movements of the build platform aiding the fusion of upcoming layers. Unsintered powder provides support to the main structure and is reused later, careful handling of the powder is always essential for safety and health reasons. SLS enables the fabrication of self-supporting structures and produces products with complex internal geometries like orthotics and prosthetics (Banga et al., 2020). The process is costly in terms of the economy of raw material and power consumption still, it's preferred over FDM, when the objective is to produce more précised products in the dental and orthopedic appliances (Javaid and Haleem, 2018, 2019a; Tagliaferri et al., 2019). (Schrank and Stanhope, 2011) performed a comparative analysis to check the dimensional accuracy of SLS-made ankle braces (AFOs) and the potential capability of the process to fabricate custom orthoses. (Harper et al., 2014) tested the gait performance results of passive dynamic AFOs (PD-AFOs) made by SLS and compared the biomechanical measures with traditionally adopted carbon fiber AFOs, despite of getting the parallel responses, SLS PD-AFOs were prescribed for better rehabilitation outcomes due to altered design possibilities. (Engineering et al., 2018) exercised an SLS fabrication approach for fabricating AFOs from virtual designs and collected the user feedback for walking utility to compare the clinical and mechanical performance against traditional orthopedic devices made by vacuum thermoforming. The results also indicated a considerable saving in the fitting time of 10–20%. (Shahar, 2020) presented a comparative discussion between various AM technologies adopted for AFOs and TM techniques used for the purpose and concluded that SLS and FDM approaches are widely preferred for fabricating customized AFOs. The study also suggested that nylon and PA are one of the most favorable thermoplastic material adopted for AFOs fabrication. The SLS provides wider opportunities for fabricating orthotic devices especially AFOs, as the tensile strength of AFOs can reach up-to 43 MPa and Young's Modulus up-to 3.9 GPa, which offers a sustainable combination of strength and stiffness (Shahar, 2020).
In some applications, an approach similar to SLS is preferred for economic fabrication of implants, in which powder layer is selectively sintered by controlled deposition of liquid binders from inkjet-head; though the accuracy is compromised for cost in such proposals. The recent advances in AMT have made it possible to fabricate the multi-material exoskeleton casts, introducing variable stiffness properties in the products through simultaneous extrusion of dissimilar photopolymers from multiple inkjet-heads and immediate treatment of layers with UV light (Silva et al., 2017; Skylar-Scott et al., 2019).
3.3. Selection of materials for orthotic fabrication
The performance efficiency of an orthotic device is concerned with the selection of adequate material during the early designing and testing phases, as the material properties got ultimately transformed into product's physical attributes, deciding its elasticity, resilience, flexibility, durability, hardness, density and temperature response (Vaish and Vaish, 2018). The material selection analysis for orthotics can't always be dependent on a single physical attribute of the product, as a deciding factor for the material selection (Paton et al., 2007). If a material is selected only for its hardness, it will definitely not deliver the expected biomechanical performance at the desired comfort level. Rather than using plaster bandages as in TM, composites, thermoplastics, and foams are repetitively used in AM for fabricating customized orthotic devices economically (Barrios-Muriel et al., 2020). Some of the most common thermoplastic materials frequently used for the clinical utilities in orthotics are polylactic acid (PLA), ABS, PA and nylon (Shahar, 2020). The bioplastic PLA is getting significant appeal in the medical industry, as it is a biodegradable material that is prepared using renewable resources like wooden starch, corn starch and cassava which makes it the primary natural 3D printable raw material (Adekomaya et al., 2020; R. Kumar et al., 2018). Similarly, the demand of ABS for the orthotic utility always remains high as it is a low melting thermoplastic that can be easily recycled and reshaped without any chemical degradation and harmful health issues as it doesn't have any toxic carcinogens. The high tensile strength of ABS enables the fabrication of consistent and reliable orthotic devices capable of bearing adverse physical impacts under dynamic working conditions and also offers resistance to corrosive chemicals, enhancing the product's durability (Rodríguez-Panes et al., 2018). Depending upon the design features (wall thickness) and printing parameters (infill density, fill pattern) different kinds of rigid and flexible orthotic devices can be manufactured using these thermoplastics (D. Yadav et al., 2020).
Soft foam materials constitute the flexible part of the orthotic devices with open or closed cellular structures to facilitate the ventilation and prevention of the sweat penetration to aid the user's comfort, which is unexpected in traditionally made plaster castings (Rome, 1991; Sanders et al., 1998). (Paton et al., 2007) tested the physical properties (stiffness, resilience, density, durability and static coefficient of friction) of the fifteen most commonly used soft materials in orthotic fabrication and ranked them with an indicator score for their performance in preventing diabetic foot ulcers. The study revealed that for damping the mechanical stresses in orthotic therapy, the most appropriate materials are Poron@96 (6 mm thick) and Poron@4000 (6 mm thick), and ethylene vinyl acetate (EVA) is clinically desirable due to its properties for providing the best motion control. The recent development in the AMT has enabled the fabrication of soft material diabetic foot insoles with varying porosity and adjustable modulus of elasticity, for meeting the clinical demands of diabetic patients like ulcer inhibition by regulatory distribution of stresses between the foot and 3DP flexible porous insoles (Ma et al., 2019).
In SLS-based manufacturing, polyamides, composite materials, elastomeric thermoplastics and advanced nylons are frequently used for customized parts fabrication. (M.C. et al., 2008) revealed the AM process feasibility for fabricating customized PD-AFOs using nylon-based SLS materials for clinical applications to improve walking ability. The evaluation results concluded that RilsonTMD80 (Nylon 11) has shown the best damping characteristics (over nylon 12 & glass-filled nylon 12) with maximum allowable deformation and opted typically for minimal frictional energy dissipation with ease of releasing stored elastic energy. (Walbran et al., 2016) compared stress-strain behavior of different AFOs models loaded with adjustable carbon fiber spring, made using SLS with nylon, FDM with PLA, and FDM with carbon-filled PETG (polyethylene terephthalate). The outputs revealed that none of the nylon samples attained fracture point up to 5% of strain, showing highly flexible behavior and suggested for being used in fabricating single piece AFOs. The values of yield stress for the carbon-filled PETG sample and PLA sample were close in range and recorded as 97 MPa & 88 MPa, and the PLA was opted for the utility due to its higher fracture strain and low cost of printing. It is a considerable remark that composite materials have shown the best compatibility for producing multi-functional orthotic devices by enabling lightweight, strengthened, comfortable, rigidly flexible and aesthetic design fabrication (Shahar et al., 2019).