1. Introduction
Buccal route offers several advantages than oral route [1] due to the high total blood flow which ensures systemic bioavailability, avoiding first-pass hepatic metabolism and gastrointestinal drug degradation [2]. Moreover, it is easily accessible for administration by patient and suitable for dosage forms administration and removal. However, the accidental swallowing of delivery systems and the continuous dilution by saliva could determine a low residence time of formulation in buccal cavity and, consequently, a low drug bioavailability [3]. For this reason, various bio(muco)adhesive polymers which can establish a strong adhesive contact with the buccal mucosa, allowing one to increase residence time of delivery systems and to optimize drug bioavailability [4], [5].
Polymers have been related to drug delivery systems [6], especially buccal drug delivery [7], [8], [9]. Some structural characteristics for polymers include: strong hydrogen bonding groups, strong anionic or cationic charges, high molecular weight, chain flexibility, and surface energy properties favoring spreading on a mucus layer [10], [11], [12].
A wide range of polymers, both natural and synthetic, have been studied for their potential use as mucoadhesives (Table 1). The polymers that adhere to the mucin surface can be conveniently divided into three broad categories: 1) polymers that become sticky when placed in water and owe their bioadhesion to stickiness; 2) polymers that adhere through nonspecific, noncovalent interactions that are primarily electrostatic in nature (although hydrogen and hydrophobic bonding may be significant); 3) polymers that bind to specific receptor sites on the cell surface [10], [13], [14].
Table 1. Mucoadhesive polymers in buccal delivery.
| Criteria | Categories | Examples |
|---|---|---|
| Source | Semi-natural/natural | Agarose, chitosan, gelatin |
| Hyaluronic acid | ||
| Gums (guar, hakea, xanthan, gellan, carrageenan, pectin, and sodium alginate) | ||
| Synthetic | Cellulose derivatives: CMC, thiolated CMC, sodium CMC, HEC, HPC, HPMC, MC, methylhydroxyethylcellulose | |
| Poly(acrylic acid)-based polymers: Carbomers, PAA, polyacrylates, poly(methylvinylether-co-methacrylic acid), poly(2-hydroxyethyl methacrylate), poly(acrylic acid-co-ethylhexylacrylate), poly(methacrylate), poly(alkylcyanoacrylate), poly(isohexylcyanoacrylate), poly(isobutylcyanoacrylate), copolymer of acrylic acid and PEG | ||
| Others: Poly(N-2-hydroxypropyl methacrylamide) (PHPMAm), polyoxyethylene, PVA, PVP, thiolated polymers | ||
| Aqueous solubility | Water-soluble | HEC, HPC (water < 38 °C), HPMC, PAA, sodium CMC, sodium alginate |
| Water-insoluble | Chitosan (soluble in dilute aqueous acids), EC | |
| Charge | Cationic | Aminodextran, chitosan, dimethylaminoethyl (DEAE)-dextran, trimethylated chitosan |
| Anionic | Chitosan-EDTA, CMC, pectin, PAA, sodium alginate, sodium CMC, xanthan gum | |
| Non-ionic | Hydroxyethyl starch, HPC, poly(ethylene oxide), PVA, PVP, scleroglucan | |
| Potential bioadhesive forces | Covalent | Cyanoacrylate |
| Hydrogen bond | Acrylates [hydroxylated methacrylate, poly(methacrylic acid)], PC, PVA | |
| Electrostatic interaction | Chitosan |
CMC: carboxymethyl cellulose; HEC: hydroxyethylcellulose; HPC: hydroxypropyl cellulose; HPMC: hydroxypropyl methylcellulose; MC: methylcellulose; PAA: poly(acrylic acid); PVA: poly(vinyl alcohol); PVP: poly(vinyl pyrrolidone); EC: ethyl cellulose; PEG: polyethylene glycol; EDTA: ethylenediamine tetraacetic acid.
For application to buccal mucosa, polymers may have desirable characteristics, such as: polymers and its degradation products should be nontoxic; it should not irritate the mucous membrane; the polymer should allow flexibility and comfort of the dosage form; it should adhere quickly to moist tissue and should possess some site specificity; and it should allow easy incorporation of the drug and offer no hindrance to its release [12], [15], [16].
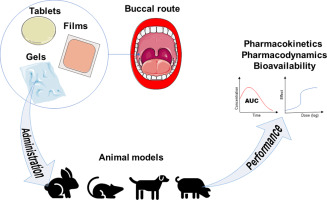
This review summarizes the applications of polymers for designing of dosage forms for buccal route, with emphasis on in vivo performance studies, which are pharmacological, pharmacodynamic and pharmacokinetic studies.
2. Buccal drug delivery
The release of drugs for the buccal route has gained great interest in Pharmacy and Materials Science [3], [17]. This interest has increased because the oral route compared to oral administration, and it has more advantages and maximizes the therapeutic potential of drugs [18], [19]. Drugs administered by the buccal route not show pre-systemic metabolism, however, it happens in the gastrointestinal tract, as well as the first pass metabolism in the liver after absorption to the bloodstream [18].
The main challenge for the success of buccal release is the residence time of the dosage forms in the oral environment. The dosage forms need to maintain contact with the mucous membrane to allow the drugs to act at the buccal site, or to be absorbed through the mucosa. However, the shearing in the oral environment, caused by saliva flow, chew, swallow, speech, may prevent adhered to the oral mucosa and this leads to a reduction or no efficacy of drugs [18], [20], [21].
A buccal mucosa covers the inside of the cheek, as well as an area between gums and upper and lower lips [22] and has an average surface area of 100 cm2[19]. Mucosa has a function to protect underlying tissues from mechanical and chemical damage [19].
The anatomy of the buccal site consists of three types of mucosa: the mucous membrane lining found outside the oral vestibule, the sublingual region and the specialized mucosa. The specialized mucosa is found on the dorsal surface of the tongue, while the masticatory mucosa is found on the hard palate and gums [21]. The mucous membrane lining comprises about 60%, the masticatory mucosa approximately 25%, and the specialized mucosa approximately 15% of the total surface area of the oral mucosa in an adult human [23]. Fig. 1 shows a schematic representation of oral cavity.
 Fig. 1. Schematic representation of oral cavity and buccal mucosa histology.
Fig. 1. Schematic representation of oral cavity and buccal mucosa histology.The masticatory mucosa is located in regions particularly sensitive to stress from chewing activity. The cells of the masticatory mucosa are keratinized and a lamina propria connects the mucosa to the periosteum. The mucous membrane lining, on the other hand, is not so subject to these masticatory shears and, consequently, has a non-keratinized epithelium, and a thin and elastic lamina attached to submucosa. The mucosa present in the dorsum of the tongue is a specialized mucosa and surfaces embedded with numerous papillae and taste receptors [23]. Schematic representation of oral mucosa histology is shown in Fig. 1.
The mucosa thicknesses range from 500 to 800 μm for a buccal mucosa and for a sublingual and gingival mucosa, thickness values between 100 and 200 μm [24]. The nature of the epithelial mucosa varies according to tissue function, but in general it functions as a barrier to lipophilic drugs [24]. Saliva is a moderately viscous aqueous fluid secreted by the parotid, submandibular and sublingual glands [25]. A salivary film is distributed over the mouth surfaces, coating the epithelial cells and tooth enamel [26] and the thickness of this film is about 70–100 μm [23].
The major components of saliva are mucus, proteins, minerals and enzymes. Saliva is considered a weak buffer system with a pH of 5.5–7, and the pH range depends on the composition and ionic composition that are affected by the type and degree of stimulation (smell, taste, and type of food). The normal salivary flow rate is approximately 0.5 mL min− 1, resulting in daily secretion between 0.5 and 2 L, but due to continuous swallowing, the constant volume of saliva in the mouth is approximately 1 mL [18], [19].
Mucus is composed mainly of glycoproteins which are called mucins, which are macromolecules with a molecular weight between 0.5 and 20 MDa [27]. Slomiany et al. [28] reviewed the molecular aspects of salivary mucins and the nature of oral mucosa interactions with mucin. The negative charges of the mucins, in physiological pH values, result of ionization of sialic acid and sulphate residues. These negative charges allow the mucin to attach to the surface of epithelial cells, forming a gel layer on the surface of the epithelium. In aqueous media, the mucins molecules are complexed gelling systems and that are stabilized by intra- and intermolecular hydrogen bonding, electrostatic interactions and disulfide bonding between the cysteine residues present in non-glycosylated regions [29]. The amount of disulfide bond present in the mucins influences the their viscoelastic behavior [30].
Paderni et al. [31] reported that administration of drugs through the buccal mucosa can be subdivided into two different approaches that may result in a local or systemic effect. This variability results from the regional differences in terms of anatomical characteristics and permeability of each anatomical site [31], [32]. The keratinized mucosae present in the gingival and hard palatal are not considered a site for systemic administration and are these mucosae is considered useful sites for the local delivery of drugs in the treatment of oral diseases located in the gingiva or palate [31], [33].
The administration through the non-keratinized mucosa can be subdivided into two approaches: sublingual delivery or delivery through the buccal mucosa [31]. The sublingual mucosa is more permeable and has high vascularization and thinner than the buccal mucosa, and it shows a viable site for rapid onset for the absorption of drugs [34]. Thus, the sublingual route is generally used for systemic delivery in the treatment of acute disorders (angina pectoris or acute pain). However, the surface of this mucosa is constantly washed by the saliva and the shear exerted by the tongue makes it difficult to maintain the dosage form in contact with the mucosa [34].
The cheeks mucosa is less permeable, and unable to provide a rapid onset of absorption when compared to the sublingual mucosa; however, it may have local or systemic effects when drugs are administered [1], [31]. The surface of the buccal mucosa is relatively immobile and more permeable than the other tissues of the oral mucosa. Thus, it becomes a place of choice for the administration of controlled release systems that need to be adhered for an extended period [34].
Transport of drugs through the transcellular pathway, also known as the intracellular pathway, may occur by diffusion to low molecular weight molecules or by active transport, also known as facilitated diffusion, to polar or ionic compounds; or by endocytosis and transcytosis for macromolecules [35].
The transport of molecules through the intracellular pathway is a complex phenomenon that is dependent of physicochemical proprieties of the drugs, such as molecular weight, oil/water partition coefficient, ionic charge and structural conformation. Lipophilic compounds and small hydrophobic molecules predominantly pass through by intracellular transport [24]. These transport pathways are shown in Fig. 2.
 Fig. 2. The drug transport mechanism through the buccal mucosa involves two major routes: transcellular (intracellular) and paracellular (intercellular) pathways.
Fig. 2. The drug transport mechanism through the buccal mucosa involves two major routes: transcellular (intracellular) and paracellular (intercellular) pathways.Cell membrane is lipophilic, for hydrophilic drugs have difficulty to permeating the cell membrane. The passive transport of hydrophilic compounds, including macromolecules, such as peptides and proteins, may be enhanced by the interaction of the excipients of the formulation with the phospholipid bilayer and the integrated membrane proteins [35]. In the case of lipophilic drugs, the lipid bilayer performs the pathway and, for hydrophilic drugs, there is an interaction associated with the aqueous regions adjacent to the polar groups of the phospholipid head present in the lipid bilayers [36]. Water-soluble solutes, such as amino acids, ions and sugars, can be diffused through the pores present in cell membranes [35].
Although the buccal mucosa as a novel drug delivery route is being widely explored recently, its potential as a route for drug delivery was known to mankind centuries ago. Modern day researchers are therefore exploring the various routes available for drug delivery, especially through the oral mucosa, and coming up with novel drug delivery systems: tablets, films, patches, gels and nanotechnology-based systems (Table 2).
Table 2. Summary of drug delivery systems suitable for buccal route.
| Systems | Composition | Drug or ingredient active | Major results | Model | Reference |
|---|---|---|---|---|---|
| Hydrogels | Chitosan | Doxycycline and meloxicam | Improvements in clinical score | Dog | [37] |
| Carboxymethyl cellulose | Dextrose | Gel not increased the risk of rebound or recurrent hypoglycaemia, well tolerated, and was not associated with adverse effects | Randomized controlled trial in babies | [38] | |
| Chitosan with/without cetrimide | Peptide HsTX1[R14A] |
Good results in in vitro mucosa permeation Peptide was detected in plasma Presence of cetrimide in the gel further enhancing plasma exposure |
Swiss mice | [39] | |
| Polycarbophil and poloxamer 407 (gel matrix) and others excipients | Curcumin | High rate of healing, effective pain index and reduction in lesion size | Volunteers (clinical) | [40]b | |
| Carbopol 71G gela loaded-microemulsionb | Simvastatin | Improved buccal permeation and pharmacokinetics parameters | Albino Wistar rats | [41] | |
| Chitosanc | Toluidine blue O |
Gel enhanced drug mucosa retention Number of apoptotic cells was greater compared the controls |
Swiss mice | [42] | |
| Chitosan | Stichodactyla helianthusneurotoxin | AUC of peptide was high when associated with cetrimide | Mice | [43] | |
| Ethyl cellulose-coated modified chitosan patches | Lidocaine | Serum concentration of drug was much higher from hydrogels made with modified chitosan compared to unmodified chitosan | Rabbits | [44] | |
| Microemulsion-loaded N-succinyl chitosan geld | Eugenol, honey and sodium hyaluronate | High tissue regeneration activity | Wistar rats | [45] | |
| Linseed mucilage and chitosan | Venlafaxine | Increased of bioavailability by buccal route | Rabbits | [46] | |
| Modified-poloxamer 407 and Carbopol 934P | Triamcinolone acetonide | Inflammatory response in the mucosa was milder compared to controls | Rats | [47] | |
| Chitosan | Domperidone and mosapride citrate | Improved of bioavailability of drugs | Humans | [48] | |
| Carbopol 940 and poloxamer 188 | Loratadine-loaded transferosomes |
Gels remained in the mouth of volunteers Reduced absorption rate and AUC compared to market oral dosage form (tablets) |
Humans | [49] | |
| Carbopol 974 P NF and HPMC K 100M | Cyclosporine-loaded SLNd |
Distribution in mucosa layer of rats Improvement of wound healing |
Rats Rabbits |
[50] | |
| Cress seed mucilage and Carbopol 934 | Venlafaxine | Improved of bioavailability by buccal route compared to oral route | Rabbits | [51] | |
| Sodium carboxymethylcellulose | Buprenorphine | Pharmacokinetics of drug administered intravenously or buccal transmucosally are similar | Dogs | [52] | |
| HPMC E15 LV and Carbopol 934P | Glibenclamide | Gels successfully prevented severe hypoglycaemia, showed sustained action, and enhanced relative bioavailability | Rabbits | [53] | |
| Chitosan glutamate | Lidocaine hydrochloride | The anesthetic activity of hydrogels was assessed compared to commercial semisolid formulations containing the same drug. | Humans | [54] | |
| Poloxamer-407, HPMC K15M and methyl vinyl ether/maleic anhydride copolymer (Gantrez™ S-97) containing or not sodium tauroglycocholate | 5-Fluorouracil | The absolute bioavailability of drug from mucoadhesive gels containing sodium tauroglycocholate increased 1.6-fold as compared to the gels containing no permeation enhancer | Rabbits | [55] | |
| Carbopol 934P | Alendronate sodium | Improvement of buccal bonne regeneration in periodontal disease | Humans | [56] | |
| Many polymers gelse | Piroxicam | Sodium alginate and HPMC gel formulations applied to the buccal mucosa were able to reducing pain level, swelling and tenderness within a period of 4 days | Patients with post-operative maxillofacial | ||
| Poloxamer 407 with or without sodium deoxycholate | Triamcinolone acetonide | Triamcinolone acetonide gels containing sodium deoxycholate as an enhancer was administered to rabbits via the buccal routes, the relative bioavailability showed about 1.59-fold compared with the control group. | Rabbits | [57] | |
| Carboxyvinylpolymer and enhancer, as glycerylmonolaurate, l-menthol and sodium caprate | 17β-estradiol |
Formulation containing glycerylmonolaurate allowed the maintenance of the plasma level No morphological changes after and before buccal administration |
Male golden hamsters | [58] | |
| Sodium alginate | Tramadol-loaded PVA microspheres |
Highest mucoadhesion time and mucin adsorption capacity Buccal administration showed the same antinociceptive activity that oral route Administration of antagonist no decrease the activity of that hydrogel by buccal route |
Wistar rats | [59] | |
| Thin films | Carmellose sodium, glycerol, polyethyleneoxide coated by ethyl cellulose and dibutyl sebacate | – |
Form a mechanical barrier under the lesion Allow extending the duration of the contact in pain perception and faster healing |
Volunteers (clinical) | [60] |
| HPMC and Carbopol (loaded nanosuspension of drug), HPMC as matrix and ethyl cellulose as backing layer | Carvedilol | Formulation improved in bioavailability (9 times), peak plasma concentration (7.3 times) and extended plasma residence in comparison to oral marketed tablet | Rabbits | [61] | |
| Chitosan and ethyl cellulose | Ondansetron | The buccal administration showed prolonged efficacy and enhanced bioavailability compared to the oral solution | Hamster | [62] | |
| Polycarbophil and Eudragit S-100 | Salmon calcitonin |
The relative bioavailability for rabbits treated with the films was 43.8 ± 10.9% Plasma calcium levels after administration of drug by both the intravenous and buccal route were comparable. |
Rabbits | [63] | |
| Chitosan and polyvinyl alcohol | Vitamin B12 (cyanocobalamin) | Bioavailability of drug was increased compared to a market formulation for i.v. administration | Rabbits | [64] | |
| Eudragit L and Eudragit S | Ketoprofen | Improve clinical scores of oral mucositis | Rabbits | [65] | |
| HPMC and Eudragit® | Selegiline-loaded nanospheres | Improved bioavailability | Rabbits | [66] | |
| HPMC, Carbopol 940 and Eudragit® NE 40 D | Prednisolone | Greater bioavailability compared to oral suspension | Rabbits | [67] | |
| HPMC E5 LV | Domperidone |
Bioavailability from the buccal film was 1.5 times higher Ex vivo-in vivocorrelation was found |
Humans | [68] | |
| Sodium carboxymethyl cellulose and hydroxypropyl cellulose (HPC). | Diltiazem hydrochloride | AUC were higher for buccal administration | Humans | [69] | |
| Carboxymethylcellulose and Carbopol 940P | Salbutamol sulphate |
Prolonged effect of bronchoprotection Low rate of tolerance effect of drug |
Guinea pigs | [70] | |
| Chitosan-ethylenediaminetetraacetic acid | Insulin |
Hypoglycemic effect following buccal administration of films No toxic effect was found in the mucosae |
Rats | [71] | |
| HPMC | Rivastigmine | Excellent trans-buccal permeation and buccoadhesive characteristics with improved bioavailability | Rabbits | [72] | |
| Tablets | Co-spray-dried drug and chitosan | Diazepam | Bioavailability was at the same level observed following buccal administration of a commercially immediate release tablet | Mini-pigs | [73] |
| Alginate and excipients | Ritodrine hydrochloride |
Absorption was more prolonged High mucoadhesive properties leads to superior retention of drug |
Rats | [74] | |
| Sodium alginate, HPMC and excipients | Omeprazole | Absolute bioavailability was 30% | Hamsters | [75] | |
| Alginate and excipients | Ritodrine hydrochloride | Formulation affects to drug release profile and this act on absorption rates | Rats | [76] | |
| Carbopol 934P; HPMC K4M, ethyl cellulose (cup) and sodium alginate (core) | Buspirone |
Tablet adhered to the buccal mucosa for 8 h Bioavailability was 5.6 fold greater compared to the oral commercial tablets |
Humans | [77] | |
| Spray-dried microspheres, Carbopol 934 P, ethyl cellulose and hydroxypropyl cellulose | Carvedilol-loaded chitosan microspheres |
Pharmacokinetic studies showed significantly higher than carvedilol oral tablet Pharmacodynamic studies confirmed reduction in mean arterial pressure and heart rate |
Rabbits | [78] | |
| Carbopol 934, HPMC K4M, HPMC K15M | Sumatriptan succinate | Improved bioavailability compared to oral solution | Rabbits | [79] | |
| Carbopol 971P and HPMC K4M | Felodipine and pioglitazone | Improved bioavailability of both drugs compared to oral suspension | Pigs | [80] | |
| Mucilage isolated from Dillenia indica | Oxytocin | Improved bioavailability compared to oral solution | Rabbits | [81] | |
| Chitosan and Carbopol 974P | Nicotine | No significant difference was found between the maximum plasma nicotine | Humans | [82] | |
| Chitosan with sodium alginate | Chlorhexidine | Drug in saliva showed the capacity of these formulations to give a prolonged release of the drug in the buccal cavity | Humans | [83] | |
| Microsphere | Alginate and chitosan | Nystatin |
Amount of drug in mucosa was between 4 and 6 times higher than the MIC No changes of buccal tissue |
Pigs | [84] |
- a
-
Gel containing glycerine and polyethylene glycol 400 as umectant.
- b
-
Microemulsions composed of α-Linolenic acid as the oil phase with Kolliphor EL 40 as surfactant and Transcutol HP as surfactant and co-surfactant, respectively.
- c
-
Microspheres was coated with chitosan.
- d
-
Composition: Compritol 888 ATO, poloxamer 188 and Tween 80.
- e
-
HPMC; HPC; sodium alginate; methylcellulose; HEC; Carbopol 934; NaCMC; Pluronic F-127; PVA.
3. Mucoadhesion theories
Bioadhesion can be defined as the state in which two materials, at least one of which is biological, are held together for an extended period of time by interfacial forces [17], [85]. Bioadhesive systems applied to mucous membranes are often defined as mucoadhesive, but the use of these terms may be interchangeable [86].
Mucoadhesive systems can be defined as those that bind the molecules of the mucus layer, but in reality it is difficult to discern whether the interaction occurs on the cell surface or between the molecules of the material and the mucus layer [87].
The mechanism of adhesion of certain molecules on the surface of a tissue or mucosa is not yet very well understood. The mucoadhesive pharmaceutical form should spread on the substrate to initiate a contact with the surface, promoting the diffusion of its chains into the mucus. The forces of attraction and repulsion arise, and for the occurrence of mucoadhesion, there must be a predominance of attraction forces [85].
Thus, the mucoadhesion process is generally divided into two stages, the contact the consolidation stage, both shown in Fig. 3. The first step is characterized by the contact between the material and the mucous membrane, where will occur the spreading and swelling of the formulation, initiating a contact with the mucus layer [88]. In the next step, in the consolidation phase, the mucoadhesive materials initiate a molecular interaction with the mucus by a van-der-Waals forces or hydrogen bonds [85].
 Fig. 3. The two stages in mucoadhesion.
Fig. 3. The two stages in mucoadhesion.There are two theories that explain the consolidation step: diffusion and dehydration theory. According to the theory of diffusion, mucoadhesive molecules and the mucus glycoproteins interact mutually by interpenetration of their chains and the supramolecular interactions [85]. This mechanism is shown in Fig. 4.
 Fig. 4. Secondary interactions resulting from interdiffusion of bioadhesive polymer chains and mucins of mucus.
Fig. 4. Secondary interactions resulting from interdiffusion of bioadhesive polymer chains and mucins of mucus.
Diffusion theory tends to happen with the mucoadhesive device has characteristics that favor the interactions, both chemical and mechanical, with the mucus. Molecules with functional groups that can interact hydrogen bonds (OH,  COOH), anionic surface charge; or flexible chains of polymers, can interact and penetrate the mucus layer [89]. The molecular structures of main polymers presented in this article are shown in Fig. 5.
COOH), anionic surface charge; or flexible chains of polymers, can interact and penetrate the mucus layer [89]. The molecular structures of main polymers presented in this article are shown in Fig. 5.