1. Introduction
The care and rehabilitation of individuals after lower limb amputation presents a substantial and growing socioeconomic challenge. The International Society for Prosthetics and Orthotics reports that there is a recognized need for advanced technology in prosthetic limb componentry and its provision, and there is a desire in the clinical community to enhance evidence-based practice [1].
Rehabilitation after amputation commonly aims to restore functional independence through promotion of ambulation using a prosthetic limb. Fitting a conventional prosthetic limb employing a socket for suspension commonly requires an iterative and labor-intensive process [2], [3]. This is partially a consequence of changes in the residual limb soft tissues, including their volume, shape, tissue composition, sensitivity, and scarring from surgical wounds. These factors may vary during the course of a day due to temperature, activity and hydration, or over several months, as postoperative oedemasubsides, muscles atrophy and soft tissues remodel to enable socket-skeleton load transfer [4], [5], [6].
The extent and duration of comfortable load transfer to the residual limb changes during rehabilitation, and there are considerable challenges in identifying physiologically-informed biomechanical targets for the socket's design. Instead, prosthetists aim to produce an acceptable definitive socket by using their experience and patient feedback with iteratively adjusted trial sockets. Short term changes in the residuum are typically managed using socks and soft ‘Pelite’ polymer foam or silicone gel liners. However, ill-fitting sockets are still common for this population, affecting an individual's quality of lifethrough discomfort and functional limitations, causing secondary musculoskeletal conditions such as osteoarthritis, osteoporosis, and lower back pain [7].
In below knee amputation (BKA) surgery, a soft tissue pad is created over the resected tibia and fibula comprising the gastrocnemius and soleus muscles. The pad is sutured to the anterior tibial periosteum or the bone, and a posterior or skewed flap of skin seals the site. When a conventional, socket-suspended prosthesis is used, the muscles, predominantly subject to tensile loading along the fiber direction, are therefore subject to shear and transverse compression. Strain concentrations are also experienced around bony prominences, such as the anterior edge of the tibia. Furthermore, the soft, relatively non-load bearing skin covering the calf, patella tendon, tibial plateau and anterior tibial surface becomes the primary load transmitting interface, and experiences substantial cyclic pressure and shear. In above knee amputation (AKA), similar changes in loading may be experienced by the skin and adductor muscles at the distal femur, and by the proximal soft tissues around the ischiopubic ramus and greater trochanter bony prominences. Alternatively, a prosthetic limb may be suspended by an implant, fixed directly to the residual bone by osseointegration(OI).
The residuum–prosthesis interface is the site at which the majority of early complications are observed during rehabilitation, and is directly influenced by the custom-designed prosthetic socket, liners and socks, and how they are used. The incidence of skin disorders is substantial [8], resulting from the requirement to transmit elevated compressive and shear forces between the prosthesis and residual limb. The residuum tissues are not used to bearing normal compressive and shear load, as the plantar tissues in the foot are [9], [10]. Incorrect socket fit can potentially lead to dermatologic problems such as contact dermatitis [8] and keratosis [11], and in serious cases, internal tissue strain and ischemia can lead to deep tissue injury [12]. Discomfort and the risk of skin breakdown are elevated with a moist climate due to perspiration, and prolonged exposure to the chemical compounds of the prosthesis [13]. These problems can arise in established residual limbs with no history of skin problems as a result of changes in liner and socket prescription, as well as the environment at the interface. For example, the process by which patients apply a liner to their residual limbs prior to donning a socket may introduce trapped air, which can influence skin friction, temperature and potentially lead to blistering [14].
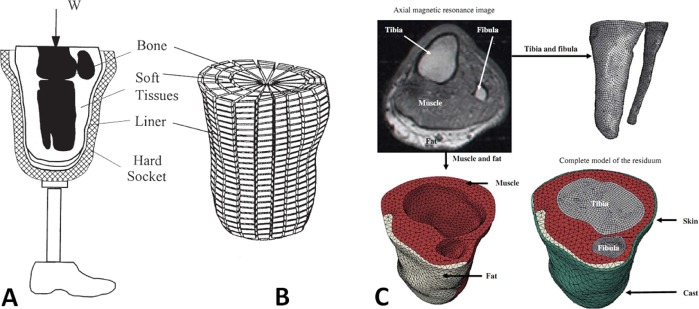
The residuum tissues must adapt to their changed mechanobiological duties, which is a lengthy and uncomfortable process. Important progress has been made towards understanding the tissues’ sustainable threshold levels of strain magnitude and duration [15] the adaptive processes are highly variable, and not fully understood. Finite element analysis (FEA) is a type of numerical modeling which, when applied to the residual limb (Fig. 1) has potential to offer insights into soft tissue load distributions and magnitudes, which may provide an evidence base to assist prosthetists with socket design, allowing rehabilitation to be expedited with reduced discomfort and treatment expense [16]. It also enables pre-clinical analysis of novel prosthetic componentry, such as OI implant-suspended concepts.
 Fig. 1. Examples of published residual limb FE models, intended to represent loading through a prosthetic socket and liner with multiple bone models (A,B), and to represent an upright-MRI scan scenario loading through a plaster cast (C). Reproduced from: A,B) Reprinted from [26] with permission from Elsevier (license 3,973,140,409,695), and C) Reprinted from [46] with permission from Elsevier (license 3,973,140,811,893).
Fig. 1. Examples of published residual limb FE models, intended to represent loading through a prosthetic socket and liner with multiple bone models (A,B), and to represent an upright-MRI scan scenario loading through a plaster cast (C). Reproduced from: A,B) Reprinted from [26] with permission from Elsevier (license 3,973,140,409,695), and C) Reprinted from [46] with permission from Elsevier (license 3,973,140,811,893).This paper reports a systematic review of the literature, up to January 2017, considering the application of FEA methods to analyze the residual tissues in the amputated lower limb, and their interface with prosthetic componentry, nominally sockets, liners and osseointegrated implants. The review's objective was to identify the state of the art in numerical analysis considering recent trends in modeling approaches and objectives, experimental validation, interface models, tissue material models, derivation of anatomic geometry, and applied loading and boundary conditions. Furthermore, the range of study questions and model output measures was evaluated, and a discussion of future research possibilities is proposed. In order to facilitate this work, reference is made to a range of clinical reports which may provide appropriate model input data or be employed for modeling corroboration, and measurement techniques for validation. Finally, comments are made regarding the potential for practical implementation of these techniques to answer the prosthetic and orthotic community's needs.
2. Methodology
2.1. Search strategy
This systematic literature review employed the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) approach [17]. Two databases (Web of Science and PubMed) were searched for relevant articles using the following keywords:
(finite element) AND ((transtibial OR trans-tibial OR below knee) OR (transfemoral OR trans-femoral OR above knee) OR disarticulation) AND (amput*)
For each article, the reference lists and forward-citation reports from each database were consulted in order to identify additional relevant articles that were not found in the automatic search.
2.2. Study selection
Primary eligible articles were selected from the full list of automatically retrieved articles. This review aimed to capture original research involving finite element analysis of the residual lower limb following amputation. Therefore, review articles, and duplicate articles published as conference proceedings were excluded. Studies which performed FEA on the prosthesis without modeling the residual limb were excluded, but the search was not restricted to any particular prosthetic componentry type. Finally, studies were assessed for their methodological and results detail. Articles were excluded which did not offer quantitative details of material properties, loading and/or results. Triangulation between the three authors was used to verify the decisions to exclude articles.
Where the full text of an article was not available, the corresponding author was contacted by their current email address. A small number of non-English-language articles were identified, and again the corresponding author was contacted and a translated version, or an interpretation of the key study information was requested. In both situations, if no response was received within one month, the study was excluded.
Finally, in light of past reviews conducted on this subject, the search was restricted to studies published from the year 2000 onwards. Silver-Thorn et al. [18], and Zachariah and Sanders [19] produced reviews in 1996 including detailed analyses of prior FE modeling approaches, which were followed two years later by Zhang, et al. [20]. More recent review articles [21], [22], [23], [24], [25] have considered finite element analysis of the residuum and prosthesis as part of a wider remit, but provided valuable insight into the state of the art and scope for further research, which are presented in the Discussion section.
3. Results
3.1. Search results
On 14th September 2016, the automated search identified 92 articles in the Web of Science database, and 63 in the PubMed database. After screening to the eligibility criteria listed above, 39 eligible articles remained. Two more articles were excluded because they did not include sufficient details for full assessment. Through review of the eligible articles’ reference lists and forward citation lists, a further 8 eligible articles were identified, giving a total of 45 articles (Fig. 2). The search was repeated one month later, and again on 1st January 2017 during the response to reviewers’ comments, and no additional articles were identified.
 Fig. 2. Literature search process and results.
Fig. 2. Literature search process and results.3.2. Grouping
The articles were grouped by intervention (Fig. 3). The search yielded 25 articles on transtibial amputation since year 2000: [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50]), 4 articles on conventional transfemoral amputation since 2000: [51], [52], [53], [54]), and 16 on transfemoral amputation treated with an osseointegrated prosthesis since 2000: [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70]). The search was robust against variants including ‘exarticulation’ and ‘through-knee’ in place of ‘disarticulation’. The main observed trends in publication were a greater focus upon transtibial than transfemoral amputation, and a recent increase in osseointegrated prosthesis modeling, applied to AKA.
 Fig. 3. Articles and publication years sorted by intervention. BKA (below knee amputation); AKA (above knee amputation); OI (osseointegrated prosthesis).
Fig. 3. Articles and publication years sorted by intervention. BKA (below knee amputation); AKA (above knee amputation); OI (osseointegrated prosthesis).The post-2000 eligible articles were grouped by research focus into the following categories: (1) residuum–prosthesis interface mechanics (Table 1); (2) residuum soft tissue internal mechanics (Table 2); (3) identification of residuum tissue characteristics; (4) proposals for incorporating FEA into the prosthesis fitting process; (5) analysis of prosthetic componentry innovations; and (6) analysis of osseointegrated prostheses (Table 4). This grouping forms the structure of the Discussion. For each study, the pre- and post-processing parameters were identified (Fig. 4) so that trends in methodology and results could be identified.
Table 1. Characteristics of residuum-prosthesis interface mechanics models.
 |
|---|
Table 2. Characteristics of residuum soft tissue mechanics models.
 |
|---|
 Fig. 4. Methodological and results categories extracted from the identified studies, grouped by analysis input (pre-processing) and output (post-processing) parameters.
Fig. 4. Methodological and results categories extracted from the identified studies, grouped by analysis input (pre-processing) and output (post-processing) parameters.4. Discussion
4.1. Modeling residuum-liner and socket interfaces
The first group of articles studied residual limb–prosthesis interface mechanics (Table 1). Of these, the first seven (published 2000–2005) concentrated upon below knee amputation, and the last three (published 2011–2015) on above knee amputation. Lacroix and Fernandez Patiño 2011 [51] also studied the internal mechanics of the soft tissues.
The residuum–prosthesis interface was the focus of the first substantial effort in computational prosthetic biomechanics research. As a result of the clear importance of this interface, described in the Introduction, sustained work following Krouskop et al's 1987 study [71] has investigated numerically predicted interface stress as a tool to assist in prosthetic socket design (see Section 4.4). The earliest identified studies employed static loading conditions, and assumed rigid bone or prosthetic socket components in single anatomic cases. Particular contributions made by the cited subsequent studies include the generation of all anatomic geometry from single imaging modalities, model loading and boundary conditions incorporating both pre-stresses from socket donning [32] and quasi-dynamic loading [34], [36], [51], the employment of soft tissue material models capable of demonstrating nonlinear hyperelasticity [51], [53], and the assessment of inter-subject variability by simulating multiple cases [51], [54]. Prosthetic sockets have generally been represented as a rigid boundary condition, with the argument that the socket has negligible flexibility compared to the soft tissues. Comparison between the rigid-socket BKA studies and the two papers which did model the socket [27], [32] suggests that this assumption caused an elevation in interface stresses, although the effect is confounded by several factors, most notably the effects of compliant socket liners. It is argued that with present computational power, the various prosthesis socket and liner layers should all be included with representative stiffness.
Interface modeling yields limb–prosthesis pressure and shear stress outputs, which are attractive results because they relate to potentially measurable quantities, assisting model validation. These two topics formed the remit of the 1996 review by Zachariah and Sanders [19], and are updated in Section 5.4.
The choice of contact model will have a substantial influence upon limb–prosthesis interface simulations. Studies identified in the present review addressed the issues associated with large relative tangential displacements by considering contact element types that differ in their contact partner identification technique [27], and by use of explicit finite element formulations[51]. However, within the identified studies, little was reported concerning the friction model itself. Generally, a single coefficient of friction (COF) value was quoted, between 0 (frictionless) and 1 (bonded), but most commonly between 0.4 and 0.5. This indicates the use of a Coulomb ‘stick-slip’ friction model, whereby tangential force can be transmitted (stick) until its magnitude exceeds the product of the normal force and COF, when tangential relative displacement is permitted (slip). In the cited quasi-static, implicit FE models, it appears that no difference between static and dynamic friction coefficient has been considered. The majority of the cited studies refer to two experimental COF reports: Sanders et al. [72] performed static COF measurements between skin, socks, and conventional socket and liner materials, and Zhang and Mak [73]performed similar dynamic COF measurements. Necessarily, both studies cleaned the test-site skin of their participants, and conducted testing dry, at ambient temperature. Future models may consider the effects of elevated temperature and humidity, and the presence of moisture, grease or sweat at the skin surface, which have been found to have highly variable effects upon COF as reviewed by Derler and Gerhardt [74]. Most recently, Ramirez et al. [75]observed that artificial sweat and hair could produce COF values as low as 0.22, possibly by inhibiting adhesion of stratum corneum cells to the surface [72]. However, the content and quantity of surface moisture are important, and the interpretation of such models must be undertaken with care. Although sweat and sebum may, in sufficient quantities, produce lubricating effects and reduce the shear stress established in the skin, they may also reduce the threshold strains sustainable before tissue damage occurs [76].
4.2. Residuum soft tissue internal mechanics
It is now understood that pressure ulcers can develop in deep tissue adjacent to bony prominences, and may only display external signs of injury after extensive tissue damage has occurred [77]. Tissue damage may result from compression-induced ischaemia, and shear strain above a threshold level [78]. This is of particular concern in the reconstructed soft tissue pad in the amputated limb, especially early in rehabilitation, due to the combined action of cyclic and sustained compressive and shear loads and elevated temperatures experienced in tissues which are not used to load-bearing.
4.2.1. Developments in residuum internal soft tissue modeling
The primary modeling focus shifted from residuum–prosthesis interface mechanics to the internal mechanics of the soft tissues (Table 2), since approximately 2006, with notable efforts from Portnoy in Gefen's group at Tel Aviv University [43], [44], [45], [46], [49]. Again the focus was initially on below-knee amputation, and particular contributions include the improvement of model geometry and material model definitions, and the use of Open MR (magnetic resonance) imaging to characterize 3D tissue displacements under load. Two later papers considered the above-knee case [51], [52], with Lacroix and Fernandez-Patiño introducing explicit FEA formulation to simulate the large-displacement sliding scenario of socket donning. Sanders and Daly [79]reported in 1993 the interface shear stresses generated by ambulation loading, and the important element introduced by Lacroix and Fernandez-Patiño's study was the explicit simulation of socket donning, which enabled additional residual shear stress to be captured. Earlier models simulated the tissue–socket interference fit by imposing ‘overclosure’ displacement normal to the surface, and were thus only capable of generating interface compression. These are both valuable contributions to the prediction of combined interface pressure and shear stress distributions, as well as the deviatory and dilatational components of soft tissue strain. These factors will have considerable influence upon the prediction of injury risk, discussed further below.
Considering the developments in applied material models for the soft tissue structures, linear elastic simplifications have been largely replaced by models which allow hyperelasticity and, in one case, viscoelasticity, although maintaining assumptions of isotropy and within-tissue homogeneity.
The majority of the identified studies considered relatively conventional modeling output measures including maximum and minimum principal stresses and/or strains, strain energy density, and equivalent stress magnitude (commonly referred to as ‘von Mises’ stress in FEA packages). Another interesting contribution of Portnoy et al. in their 2011 paper [49] related to their model post-processing using two phenomenological deep tissue injury (DTI) rules. First, employing principles developed by Linder-Ganz et al. [80], they considered a sigmoid pressure–time threshold for muscle tissue injury based upon compressive stress:(1)where σ is a compressive Cauchy stress, t is the exposure time, and K, α, t0 and Care empirical constants from animal data. This technique was extended two years later by Gefen et al, in terms of strain [15].
Second, the study used this prediction of the cause of tissue injury to predict its progression, by implementing a time-based stiffening of damaged tissue material properties through iterative FE solutions as follows:(2)where Ginjured and Guninjured are the muscle tissue shear modulus values, and A0, A1 and A2 are empirical constants again from animal data [81]. Thus, the progressive risk of DTI could be predicted around bony prominences in the residual limb.
4.2.2. Tissue nonlinear elasticity/hyperelasticity
Linear elasticity was assumed for the soft tissue models in the earlier studies identified in this review (Table 3, 2000–2007). This is appropriate for materials that deform and recover in a linear manner in response to applied load, and according to Hooke's law this behavior can be characterized for infinitesimal strains by the Young's modulus (E) and the Poisson's ratio (− 1 ≤ ν ≤ 0.5) alone. The Poisson's ratio, the ratio of transverse to axial strain, is related to the material's compressibility. Soft tissues are commonly considered incompressible (ν = 0.5) owing to their high water content, although this limiting value can produce numerical singularities in the FEA computation, so values of ν = 0.45 − 0.49 were used by the earlier studies identified in this review. They also, however, commonly exhibit large strains and non-linear stress–strain behavior. In their 2003 indentation test and FEA study (discussed in more detail below), Tönük and Silver-Thorn [29] used a hyperelastic soft tissue model. Portnoy et al's 2008 paper [44] introduced this in a full residuum–socket model. Across the variety of sources consulted, a range of different notations have been used so the application of hyperelastic models is reproduced in Appendix, employing notation in general from Portnoy et al's work and ABAQUS, the most commonly employed finite element solver in the cited studies, for clarity.
Table 3. Employed soft tissue elasticity models (see also Appendix).
| Formulation | SED Function W | Uses in reviewed studies | Constitutive model parameters | Source | Species/Site |
|---|---|---|---|---|---|
| Neo-Hookean | Muscle [44]Scar [45] |
G = 8.5 kPa C10 = 148.9 kPa |
[91] [175] |
Porcine, Gluteus Human, Skin (Burn) |
|
| Neo-Hookean, Compressible |
Fat [45] Fat [49] Muscle [45] Muscle [49] All soft tissue [51] |
C10 = 0.143 kPa, D1 = 70.2 MPa−1 C10 = 2.97 kPa, D1= 34.775 MPa−1 Soft, Flaccid C10 = 2.3 kPa, D1 = 4.36 MPa−1 Ave, Flaccid C10 = 4.25 kPa, D1= 2.36 MPa−1 Stiff, Flaccid C10 = 6.2 kPa, D1 = 1.62 MPa−1 Contracted C10 = 8.075 kPa, D1 = 1.243 MPa−1 C10 = 4.25 kPa, D1= 24.34 MPa−1 as Ave, Flaccid Muscle in [45] |
[176] [177] [91] [91] [91] [178] [91] |
Ovine, over Gluteus Human, Breast Porcine, Gluteus Porcine, Gluteus Porcine, Gluteus Human, Rectus Femoris Porcine, Gluteus |
|
| Mooney Rivlin | W = C10(I1 − 3) + C01(I2 − 3) | All soft tissue [53]* | C10 = 85.5 kPa, C01= 21.38 kPa | [179] | Human, Plantar |
| Extended Mooney | W = C10(I1 − 3) + C11(I1 − 3)(I2 − 3) | Skin [44], [45], [49] | C10 = 9.4 kPa, C11= 82 kPa | [82] | Human, Volar Forearm |
KEY: Cij = deformation constitutive model parameter (material property); D1 = volumetric constitutive model parameter; G = shear modulus; I1, I2 = invariants of principal stretch ratios; J = total volume ratio; W = strain energy density.
- *
-
compressibility was included by stating a Poisson's ratio, which ABAQUS uses as .
Several hyperelasticity models have been employed in modeling the soft tissues in amputated limbs, which are formed from a strain energy density (SED) function W. This is expressed in terms of the deformation invariants of principal stretch ratios I1 and I2, and the total volume ratio J, which are calculated from the FEA-predicted model deformations. The SED function contains constitutive parameters Cij and D1 which are material constants, and these are obtained by empirical fit of a selected SED function's stress–strain profile to experimental data [82]. The identified studies used SED functions taken from general material characterization studies rather than model or patient-specific information. Furthermore, by necessity several of these past studies used ex-vivo animal tissue for characterization.
The identified studies employing linear elastic material models for all soft tissue, generally those investigating limb surface stresses only, eventually followed Zhang et al's 1995 [83] model of E = 200 kPa, ν = 0.49. The later identified studies, mainly those investigating internal soft tissue stresses, employed hyperelasticity (Table 3). The established approach, which has informed the majority of successive studies, was presented in Portnoy et al's 2009 residuum risk factor parameter study [45]. This used compressible Neo-Hookean models for fat and muscle, varied for several levels of stiffness and contraction, an incompressible Neo-Hookean model for scar tissue, and an incompressible extended Mooney model for skin.
A general observation across the models reported in Table 1 and Table 2 is that peak predicted limb–socket interface normal stresses under stance and gait loading were markedly higher in earlier studies. This is attributed to the earlier use of linear elastic soft tissue models (typical peak normal stresses of 200–350 kPa) with larger elastic moduli than when hyperelasticity was introduced (typically 120–260 kPa). As noted, peak internal strain is currently preferred to surface stresses in predicting tissue damage [15], so appropriate elasticity models and consideration of pre-strain from socket donning are essential.
4.2.3. Residuum thermal analysis
Finally, to return to the systematic review-identified studies, one paper was identified that conducted particularly notable internal tissue analysis in the residuum. Peery et al. [84] considered the thermal conditions in the residual limb tissues after donning a socket, and validated their models against experimental surface temperature measurements at rest. Such simulations are of future value in parallel with structural analysis, to evaluate the combined influence of mechanical deformations and elevated temperature or humidity upon the risk of tissue damage. Indeed elevated temperatures have a detrimental effect on skin by affecting its mechanical stiffness and strength [85], therefore increasing the risk of tissue damage [86]. Elevated moisture will also soften skin and increase cellular permeability leading to a greater susceptibility to skin irritation [87]. In some scenarios, moist skin will also have an increased coefficient of friction, resulting in elevated shear forces at the device-skin interface [88].
4.3. Identification of residuum tissue characteristics
4.3.1. Soft tissue model constitutive parameters
A third set of identified studies employed FEA to determine residuum soft tissue characteristics, making notable contributions of material models for nonlinear elasticity and viscoelasticity effects, representing an improvement in model fidelity. The authors inferred the soft tissues’ material properties from experimental data using the empirical, iterative ‘inverse method’. In 2003, Tönük and Silver-Thorn [29] reported soft tissue indentation tests on 7 patients, and then produced axisymmetric indentation FE models in order to identify regionally appropriate nonlinear elastic constitutive coefficients for a simplified 3-parameter James-Green-Simpson strain energy density function (see Appendix). Models were patient-specific, representing 11 locations of interest in socket rectification, with dimensions taken from magnetic resonance (MR) imaging or x-ray computed tomography (CT) scans. The models were solved with iterative modifications to the constitutive model coefficients at three displacement rates until less than 1% normalized sum of square error (NSSE) was obtained between experimental and numerical indenter forces. Coefficients were found to vary substantially between individuals and sites, and within-individual for a particular tissue site after a 20-month period. Their parameter search method was structured but manual, so may have identified local NSSE minima, which may be avoided using more automated minimization methods, or Monte Carlo approaches [89]. They extended this work to include viscoelastic effects in 2004 [33], described below.
More recently researchers at MIT published further work towards the same goal, including a robotic limb indentation device which builds a map of tissue compliance at 18 locations. This was used with inverse FEA to identify constitutive parameters of a 2nd order Ogden hyperelastic material model, incorporating viscoelasticity, by optimization [50]. It is difficult to assess the agreement between the tissue property predictions obtained from these studies due to the different material models employed. Furthermore, high variability was reported between individuals [29], [33], and marked spatial and temporal variation was observed in the properties calculated for the same individual.
4.3.2. Time dependent soft tissue properties
Time dependency of soft tissue loading in residuum FE models has received relatively little attention, although several of the experimental material property reports cited in Table 3 do present applicable data. A small subset of studies have attempted to incorporate the viscoelastic process of stress relaxation (whereby under a constant, finite strain, stress decreases), and one considered creep (where strain increases under a constant, finite stress).
Portnoy et al's 2008 paper [44] reported the use of stress predictions to infer the risk of soft tissue injury. These authors applied a Prony series expansion to represent stress relaxation [90]. The asymptotic relaxation level was defined in terms of the shear modulus at the instant of load application Gins and after relaxation G∞ by:(3)
They modified S, the second Piola − Kirchhoff stress from the FE database, by the Prony method: (4)where E is the Green Lagrange strain, δ is the magnitude relaxation parameter, the percentage difference between tissue moduli at the instant of strain initiation and after relaxation, and τ is the time constant of relaxation. They did not model the stress relaxation transient, as they were considering long-term deep tissue injury (DTI), and so simplified their asymptotic stress level to:(5)where δ was taken as 0.5 [91].
Obtaining the temporal parameters of the viscoelastic relaxation function would potentially enable researchers to represent the transient effects of stress relaxation explicitly.
Tönük and Silver-Thorn [33] used their previously reported time-independent model with a Prony series expansion and a linear Kelvin–Voigt model of viscoelasticity. They used regression between experimental and simulated indentation to fit both hyperelastic constitutive model parameters, and magnitude and temporal viscoelasticity parameters. They also considered both short and long term viscoelastic effects, and indenter force relaxation and creep data for step displacement and force responses, respectively. They noted that different viscoelastic parameters were obtained when creep and relaxation data were used. Alongside expected variations from model simplifications and experimental error, the creep and relaxation data were collected on different days, suggesting appreciable diurnal variation in tissue behavior. Sengeh et al. employed a related approach in their robotic indenter residual limb tissue compliance mapping study [50], using the two constitutive parameters of their Ogden hyperelastic model and a two-parameter viscoelastic relaxation function, and found less spatial variability in calculated properties for their test participant than Tönük and Silver-Thorn observed in their group.
Tönük and Silver-Thorn [33] acknowledged that the applied material models can only offer phenomenological representation of the underlying physiological processes which produce time-varying properties, and as noted above, different methodologies precludes comparison of the results obtained in the small number of studies in this area. There is still a need for systematic evaluation of the temporal changes in soft tissue behavior and inter-subject variability, and potential value in comparison of different nonlinear elastic constitutive models.
4.3.3. Pressure-pain tolerance thresholds
With an alternative approach, in 2005 Lee, et al. [37] used a simplified FE model of indentation in a single individual, and physical tests from 11 locations in 8 individuals, to investigate relationships between pain threshold and tolerance with indenter pressure and tissue distortion. This was conducted at below-knee residual limb locations with a range of soft tissue layer thicknesses, and for a range of subject ages, and three linear elastic soft tissue models from literature data. Local differences in pain tolerance and threshold pressure levels were observed, with highest values as expected at the mid-patellar tendon and tibial tuberosity, and lowest values at the residuum tip. Like the studies discussed above, the authors demonstrated the importance of collecting personalized data: significantly higher average pain tolerance and threshold pressures were recorded for the two youngest individuals in the study. Two years later Lee and Zhang proposed the application this technique as part of a simulation-aided socket fitting process [42], one of the long established goals of numerical simulation of the amputated lower limb, discussed below.
4.4. Proposals for incorporating FEA into prosthesis fitting and socket fit assessment
The first proposals for incorporating numerical predictions into the CAD/CAM-based prosthesis fitting approach were made in the 1980s by researchers in Texas [71] and University College London [92]. Five relevant papers were identified in this area in the present review.
The first key contribution to FEA-informed socket design incorporated person-specific, comfort-based design parameters. Wu et al. [30], and Lee and Zhang [42] both used indenter systems to characterize the local surface pressure-pain tolerance (PPT) of a single patient. As an assessment of goodness-of-fit, they then compared the PPT to FE-predicted socket contact pressures to assess the risk of discomfort. While Wu et al. assessed a socket fabricated before the study, Lee and Zhang demonstrated how the prediction of PPT could be used as feedback to guide the socket design.
Amali et al. attempted to simplify the use of FEA in socket design or pre-clinical analysis [28]. They advocated analyzing limb–socket interface stress data from FEA predictions or physical measurements using Artificial Neural Networks(ANN) in order to produce a transfer function to simplify the response to changes in complex input parameters, such as patient and prosthesis geometry and material properties. This study contributes an important proposal to reduce the computational time and expertise requirements that are likely to present barriers to clinical adoption of FEA.
To a similar goal, Portnoy et al. proposed a subject-specific method for real time DTI risk evaluation [47]. A portable monitor was developed to measure the contact force between the residuum and the prosthetic socket at the distal tip of the residual tibia. A set of equations was used to predict the soft tissue stress in this location based upon this force, measurements of the individual's anatomyfrom radiographs, and soft tissue material properties, which were validated against an axisymmetric FE model. The equations were used to calculate real-time subject-specific internal stresses and stress-time integrals for a range of walking surfaces and slopes, which were compared to a muscle cell deaththreshold level [80]. As well as computational efficiency, this study represents a notable contribution as it takes a more physiology-based approach to the socket fit design parameter definition than pressure-pain tolerance. This is likely to be safer especially for individuals experiencing diminished sensation, but relies on the collection of appropriate and specific tissue injury threshold data.
Goh et al. demonstrated how their in-house FE code could be directly integrated with a commercial CAD software package [38], comparing FE predictions with experimental measurements from pressure transducers at 16 sites on the socket. They proposed using FEA-derived interface pressure predictions to iterate socket design, and note the requirement of further work to compare the pressure values to a personalized pain or discomfort measurement, to evaluate goodness-of-fit. Studies by the Colombo group in Milan, summarized in 2010 [48] have extended this idea. A methodology was created to design, virtually test and automatically optimize the socket for an individual patient. The patient's anatomy was characterized using surface laser and MRI scanning, linear material properties for the patient's soft tissue were calculated using indenter data, and iterative socket rectifications were made digitally [93]. More recent research has proposed how the rectification might be performed automatically based on empirical rules [94] which relate the local rectification depth to local qualitative scores of soft tissue tonicity, ‘K’ activity levels and subject weight. FE modeling techniques were used as a predictor for socket performance, and the definitive socket was manufactured using rapid prototyping techniques. The Milan studies focused on methods such as artificial neural networks for identification of rectification zones, but did not note specific outcome measure targets to predict goodness-of-fit.
Drawing consensus from all these identified studies, it is likely that informed socket design will require patient-specific geometry, material properties and pressure tolerance measurements, all of which may be collected clinically. To go beyond interface pressure and take a pathophysiological approach, modeling should focus on the translation of these loads into the underlying tissues, in the form of how tissues deform under load and the implications for tissue viability. A novel automated design method should then be compared to traditional methods of socket design, to assess the value of the advanced technology and its efficacy.
4.5. Analysis of prosthetic componentry concepts
Key examples of prosthetic limb or socket mechanical design considering explicitly the effect upon the residual limb were performed for the ‘monolimb’ concept. Preclinical analysis investigated the influence of shank stiffness upon residual limb–socket interface stress, considering shank cross section shape vs. interface pressure [35], and shank wall thickness and material vs. interface pressure and shear stress [41]. Modifications to conventional socket designs have also been considered in terms of compliant features and regions of reduced wall thickness aiming to achieve local compliance for pressure relief [39].
Numerical models have some precedence for use in analysis of the prosthetic components. Several past studies have considered the mechanics of prosthetic limb components [95], and novel socket designs [96], but studies which did not also consider the residual limb were excluded from the systematic review raw search results. The boundary conditions provided to a prosthesis model are likely to be more trustworthy where the residual limb is modeled explicitly. However, the studies in this small subset were guided by the state of the art presented in Table 1, and were performed for single residuum shape cases only. For robust preclinical analysis it is important to evaluate a concept's performance across the likely range of patient anatomy and loading conditions, in order to identify worst cases or limits of clinical applicability. Furthermore, a residuum FE model employed in pre-clinical analysis of novel prosthetic concepts must be validated in use with one or more conventional prosthesis designs, especially if the concept in consideration is an extrapolation versus devices in clinical use.
4.6. Analysis of osseointegrated prosthesis concepts
As a final main use of numerical models of the amputated lower limb, the concept of osseointegrated prosthetics has received considerable attention since 2000. Developed by Brånemark et al. from dental implant fixation technology [97], osseointegration provides direct anchoring of the prosthetic limb to the residual bone. In treatment of above-knee amputation as with dental implantology, surgery is conventionally a two-stage procedure. First, an implant is placed in the residual femoral canal, the amputation site is closed, and biological fixation is allowed to establish prior to a second procedure. Approximately 6 months later the distal bone tip is exposed again, and a skin-penetrating abutment or coupler is attached [98], [99]. Compared to socket suspension, OI prosthesis suspension is argued to improve function, gait motion and quality of life [100], to reduce the number of return visits to prosthetistsand potentially the post-surgical rehabilitation cost [3]. Observed complications of OI prosthesis suspension have included early loosening, superficial infection, and occasional deep infection [101]. Bone fractures, mechanical deformation and failure of the implants have been reported [98], and periprosthetic bone remodeling is observed [60].
4.6.1. Developments in modeling the OI implant–bone construct
The first computational biomechanical investigation of osseointegrated implant geometry using numerical modeling was reported by Krouskop et al. in 1976 [102], substantially before the technology was first used to treat lower limb amputation in the 1990s. No other OI-related studies were excluded from the systematic review due to the post-2000 date restriction. The search results showed a marked increase in computational biomechanics activity in this area after 2000, with purely FEA-based biomechanics studies of OI concepts found at approximately one per year from 2005 onwards [55], [56], [57], [58], [59], [60], [61], [63], [66], [67], [68], [69] (Table 4). The research approach in this area is similar to studies on arthroplasty prostheses, and long-stemmed cementless total hip implants in particular, concentrating on: (1) implant-bone interface mechanics, with regard to fixation and loosening, (2) bulk bone strain, with regard to periprosthetic fracture, and (3) predicting the stimulus for, and then the progression of periprosthetic bone remodeling. After initial use to drive implant geometry optimization studies [55], [56], [57], [61], these factors have been compared for different clinically-used implant designs [58], [59], [63], [66], to understand their observed bone response [60], [70], and to propose new concepts [67], [68]. The cited studies have contributed developments in the range of expected implant–bone load cases, and results parameter interrogation. This has provided enhanced understanding of the short and medium term performance of existing implants, and will enable greater confidence in future preclinical analysis work. These isolated implant-bone construct models have been validated experimentally using cadaver tests and strain gauging [68]. Although not including finite element analysis, and employing a simplified implant support structure, Thompson et al have conducted full-surface experimental strain measurement techniques for assessing OI implant mechanics [103]. These techniques have promise for validation of FE models owing to their data richness compared to discreet strain gauges, with particular value in the comparative pre- and post-implantation bone strain analysis [104] which is used as an analogue of bone remodeling stimulus.
Table 4. Characteristics of osseointegrated prosthesis concept models.
 |
|---|
Starting to consider more advanced implant-bone physiology, two additional articles were identified from the Veterans Affairs Department/University of Utah, which employed FEA to investigate the bioelectric conditions in the above-knee amputated limb with the application of electrical stimulation to promote osseointegration [62], [64]. The electric field and current density in the residual limb were predicted, generated by the application of a potential difference between the OI prosthesis (cathode) and two skin-surface anodes. This represents an early but important step in bone morphology modeling. These investigations were conducted for eleven individuals displaying a range of extents of heterotopic ossification (HO), a relatively common phenomenon in blast trauma amputation and servicepeople in particular [105]. This was the first study identified in this review to address this highly complex and variable phenomenon by modeling.
4.6.2. Dynamic and abnormal loading conditions
Scope for further purely biomechanical work in this area may be focused upon dynamic and abnormal loading conditions, owing to the substantially changed stresses imposed upon the bone surrounding the implant. The dynamic loads experienced by an OI prosthesis and its fixation to the bone have been studied in detail by Frossard et al. [106] in collaboration with researchers at Sahlgrenska who developed the original OPRA prosthesis. Their results indicated the potential differences in loads and impulses generated in gait using different prosthetic limb componentry, providing valuable input data for dynamic computational models. As noted above, periprosthetic bone fracture, mechanical failure of the implant–bone interface, and of the implant and abutment components themselves, are understood to be some of the main mechanical risks associated with OI prostheses [98], especially given the high functional demands associated with the typical OI prosthesis user. One of the studies identified in this review did consider a fall load case [67], but the range of possible falling scenarios is wide, difficult to predict, and hard to reproduce in clinical studies. Researchers have attempted to reproduce falls in healthy individuals and infer corresponding loads on OI prostheses through multi-body simulation [107], and extensive analysis has been reported of an inadvertent fall which occurred during routine gait measurement [108].
4.6.3. Bone–prosthesis-soft tissue modeling
To conclude this section, Yerneni et al. 2012 [65] performed the first study to include the OI implant–bone construct and the surrounding soft tissue structures, in order to assess the skin-abutment interface mechanics. They employed simplified geometry and loading conditions to generate maximum soft tissue shear, during sliding down a seating surface, during a seating transfer or rising from seated, and analyzed the generated radial stress in the skin around the implant–bone-skin junction. Their findings contribute early but clinically-relevant insights into preparation of the residual bone to enhance implant-skin adhesion, by encouraging stress dissipation, which is proposed to protect skin integrity. Their model was, necessarily, a simplified first representation of this region of the OI prosthesis construct. However, it lays an important foundation for further work on this primary barrier to bacterial infection, which remains a significant issue in individuals with OI prostheses [98], [109], any may be of increasing importance as OI implantation by single-stage surgery becomes more common [110].
5. Areas of further interest, and recommendations
5.1. Un-investigated conditions, reconstructions and patient factors
To the authors’ knowledge, there has been little or no research into several residual bone factors. At diaphyseal amputation levels, the residual bone will have an open-ended tubular shape immediately after surgery (Fig. 5A and C), with some degree of bevelling. Radiology provides extensive evidence of long term bone adaptation including generation of spurs due to HO (Fig. 5B and D), formation of aggressive bone edges, tumor growth, and bone bruises and fracture following trauma or adverse remodeling [111], [112]. One of Portnoy's studies considered some aspects of distal tibia and fibula morphology [45], but published simulations of the causes and progression of adaptive bone remodeling were not found in this review, except where OI prostheses were used. Fundamentally, inspection of the methods reported in the cited studies indicates that solid, rigid bone models are most common. According to radiographic evidence the canal may close by establishing a neocortex (Fig. 5E). This may occur where there is exposed cancellous bone at the amputation level, but the bone morphology progression is unknown. Simple factors like this will have a substantial influence on predicted soft tissue strain.
 Fig. 5. Coronal residuum radiographs after A,B) above knee amputation for trauma, and C,D,E) below knee amputations. A,C) show an open medullary canal (white arrows); B,D) show formation of heterotopic ossification (white arrows) and aggressive bone edges (black arrows), and E) shows apparent cortex formation over osteotomy (white arrow).A, B) Reprinted from [172] with permission from Wolters Kluwer Health (licence 4054131375261), C) Sciencephoto.com (license 277,835/UNISOU09), D) Reprinted from [173] with permission from Wolters Kluwer Health (license 4026031374603), and E) Reprinted from [174], copyright © Nordic Orthopaedic Federation, with permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of Nordic Orthopaedic Federation (license LA/IORT/P8879).
Fig. 5. Coronal residuum radiographs after A,B) above knee amputation for trauma, and C,D,E) below knee amputations. A,C) show an open medullary canal (white arrows); B,D) show formation of heterotopic ossification (white arrows) and aggressive bone edges (black arrows), and E) shows apparent cortex formation over osteotomy (white arrow).A, B) Reprinted from [172] with permission from Wolters Kluwer Health (licence 4054131375261), C) Sciencephoto.com (license 277,835/UNISOU09), D) Reprinted from [173] with permission from Wolters Kluwer Health (license 4026031374603), and E) Reprinted from [174], copyright © Nordic Orthopaedic Federation, with permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of Nordic Orthopaedic Federation (license LA/IORT/P8879).Reports were limited to the most common transtibial and transfemoral amputation techniques. No analysis of bone-bridging transtibial amputations was found, although bridge fracture is understood to be a potential complication [113], [114], and no models of knee disarticulation were found [115], [116]. Considering the short- and long-term soft tissue adaptations known to occur, as suggested by Sanders in 2005 [21], no explicit consideration of muscle disuse atrophy and fatty infiltration has been made [117], which might provide evidence to support socket designs to maintain soft tissue health. Furthermore, future effort would be well directed towards mechanobiological simulations of the soft tissue healing process [118] including the influence of suturing, anisotropic soft tissue contraction, and the formation of granulation or scar tissue, also mentioned only by Portnoy et al. [45].
5.2. Loading conditions
Few of the cited studies have considered full dynamic loading conditions. Initial work on inverse dynamics from Jia et al. in 2004 [34] considering inertial effects represents the majority of citations for gait data in the present studies, in sagittal-plane 2D or full 3D. More recent 6-axis load cell gait analysis provides useful input force and moment data [119], [120], and multi-individual analysis of residuum–socket moments has been conducted by Kobayashi et al. for transtibial sockets [121] and Highsmith et al. for transfemoral sockets [122], under different loading conditions.
As noted previously, for prediction of internal soft tissue strains, the full range of loading conditions should be applied, including residual strain from donning the socket and any liners. It was observed that no studies identified in this review mentioned simulation of a compression sock, commonly worn to help manage residuum volume, although Sanders, Cagle and co-workers have recently produced extensive experimental data which may facilitate this [123], [124].
Adverse prosthetic limb loading should also be considered. Extensive work has been undertaken for OI patients whose limbs are fitted with load cells by Frossard and colleagues, including one report of fall data captured by chance [108]. Measuring or predicting such data in socket-suspended prosthetics is more difficult. Multi-body simulation work such as that by Schwarze et al. [125]will potentially enable investigation of more varied traumatic load cases which cannot be tested ethically. This requires a model of the dynamic coupling between the residuum and socket which accounts for axial pistoning and relative angular movements [126], which would not be captured in biomechanical modeling if traditional rigid body segment assumptions are made. Such a characterization of residual bone–prosthetic limb coupling could be achieved by FEA.
Recent work by Rigney, Simmons and Kark [127] has started to bring together multibody analysis of the lower limb with FEA of the prosthetic componentry, in order to provide more representative model boundary conditions for a running blade prosthesis case study. To date they have used a residual limb model with simplified cylindrical geometry in the cited report but they list a future goal of incorporating patient-specific residuum tissue geometry and mechanics.
5.3. Soft tissue modeling, and advances in imaging
A valuable target for further development in soft tissue modeling is the application of subject-specific tissue material parameters, recognizing that there will be inter-subject variations in many factors, including local damage and visceral fat content. This is especially common with diabetes and peripheral neuropathy [128] and disuse-atrophy after amputation [117], and can be characterized by fat-saturated MR imaging. Attempts may be made to characterize these properties using elastography [129], [130], [131] or by solving an inverse problem using FEA of comparative models built from unloaded and loaded MR images [89], [132]. An extensive review of dynamic MR techniques for skeletal muscle is given by Prompers et al. [133].
One group of the identified studies used viscoelasticity and hyperelasticity at the continuum level to represent a range of material and structural nonlinearities of skeletal muscle. These effects arise from the tissue's hierarchical structure of fibers and extracellular matrix, the active–passive nature of the fibers, and the lymphatic and blood flows which may have compliance effects at the organ level. The cited reports have not yet considered skeletal muscle's anisotropy, perhaps owing to its primarily tensile loading during activity. Recent developments in continuum modeling most relevant to residual limb FEA have included hyperviscoelasticity and orthotropy under compressive loading [134], and in one of their papers Portnoy et al. implicitly accounted for the short term change in muscle stiffness with activation [45] in their constitutive model parameters.
Further work may address the combined effects of viscoelastic-like behavior of tissues at the residual limb–socket construct level. This could incorporate changes in soft tissue compliance and shape due to tissue and organ level effects, such as elevated blood flow resulting from muscle activity, the effects of which can be measured in external residuum shape changes [135]. There may be scope to incorporate limb volume (unconstrained) [136], or muscle shape changes (constrained by a socket) due to the short term effects of activation. Furthermore, atrophy causes longer term changes in soft tissue shape [135] and mechanical properties. Modeling these effects may enable the loss of adequate socket fit to be predicted.
In all of the cited interface pressure studies, a single soft tissue bulk was assumed. Residuum inhomogeneity has been captured in most detail by Portnoy et al. [44], [45], [49], who separated the residuum into three soft tissue types, and assigned different constitutive model parameters to each (Table 3). Simple tissue geometry may be acceptable if prediction of tissue–prosthesis interface stresses are required, but if a study aims to characterize internal soft tissue conditions there may be value in modeling within-tissue inhomogeneity. This may be addressed both in material models and in identifying separate tissue structures, such as separate muscle compartments. One early study by Lee et al. [137] demonstrated the significant effects arising from defining separate muscle bodies in a transfemoral, 2D plane strain model, with material inhomogeneity and the possibility for intermuscular sliding. A more recent 2D model by Rohan et al. [138] considered the effects of compression stockings and muscular contraction upon the deformation of deep leg veins. In addition to these plane strain transverse section studies, 2D modeling has been used for simulations of an oblique section of transtibial residuums [43], and assuming axisymmetry of the residual femur-implant geometry [55]. These methods enable substantial savings in computational expense, as is required for real-time simulation, and high spatial resolution local to the model's region of interest. However, idealization of 3D geometry into a 2D representation is only appropriate in some cases, and there is limited scope to incorporate out-of-plane load variation. To consider macroscopic, organ-level structural effects, and the influence of load variation along and around the residuum, full 3D analysis is required. Image processing methods are reducing the computational intensiveness of such models, enabling expansion into 3D, but they may be difficult to validate. One promising approach could be the characterization of directional muscular inhomogeneity through fascicle visualization with diffusion tensor MRI [139]. This has been shown to give representative 3D muscle deformations upon activation in the gastrocnemius, by Fernandez [140]. This approach could enable more advanced muscle activation modeling than changing the material stiffness [45], and improve predictions of interfacial and internal tissue stress under dynamic conditions. Furthermore there is potential value of introducing within-tissue inhomogeneity in skin models, by consideration of the separate stratum corneum, viable epidermis and dermislayers. The range of potentially attributable material properties of these layers, and the effects of topographical features were demonstrated by Leyva-Mendivil et al. [141] and may be included explicitly (in the former case) or through multiscale modeling (in the latter), if the goal of modeling is to assess the potential for skin damage.
There is scope for further work on loading thresholds for tissue injury relating to the residual limb. Recent work by Loerakker et al. has presented more advanced strain/time thresholds for deep tissue damage incorporating load relief and reperfusion effects, demonstrated in animal DTI models under indenter loading [142], [143], [144]. This work and prior studies [77], [78], [80], [81], [90] have considered deep tissue injury, with a general focus on indentation and sustained support surface loading for people with conditions such as spinal cord injury. Linder-Ganz et al. also established that tissue stresses and strains are influenced by pathological anatomic changes, for their paraplegic seating study participants compared to a healthy group [145]. However, injury in residual limb soft tissues presents more commonly as superficial wounds and pressure ulcers [8], [9], [10], with markedly different loading and tissue characteristics. In order to evaluate soft tissue injurytolerance under these conditions, there would be value in further research with appropriate participant sub-populations, and under combined pressure and shear loading, as experienced at the prosthesis–skin interface. Both the resulting volumetric tissue strain and the host's ability to tolerate it will be affected by anatomic and tissue changes observed in diabetic disease and advanced muscle atrophy, as well as environmental factors such as temperature and humidity [13], [76]. In association with prescribed mechanical deformations, a series of robust biomarkers could be utilized to monitor tissue health to inform strain thresholds. Measures could include local skin inflammation [146], [147], ischemia [148] and lymphatic impairment [149].
5.4. Measurements for model validation
The most established interfacial force measurement systems are film pressure sensors [150], [151] and discrete force transducers [152], which were reviewed in comparison to FEA predictions by Laing, et al. in 2011 [23]. Similar piezoelectric sensors have recently been proposed as a means for obtaining signals for active prosthetic limb control [153]. These produce normal tissue loading data only, and have limitations relating to precise pressure magnitude, gradient or contact area measurement, sensitivity to temperature and duration of pressure application, and the compliance of supporting surfaces [154]. There may also be limitations in applying these sensor films onto compound-curved surfaces due to in-plane stiffness and buckling or crinkling. Triaxial force transducers provide discreet point data and enable combined measurement of pressure and shear forces [152], but in the past had markedly higher stiffness than the residuum and required socket modification with windows for sensor application.
Use of flexible, isolated normal and shear force measurement sensors would be preferable. Recently, devices have been validated for this purpose [155], [156]and first experiments conducted in an AKA socket [157]. Full-surface, high spatial resolution measurements are also desirable for FE model validation, which may be achieved using multiple sensors as described above, or textile sensors for pressure mapping [158]. Fiber Bragg Grating (FBG) sensors have also been proposed [159], and may have benefits in spatial resolution and capabilities in dynamic measurement, although the complexity and cost of peripheral equipment may preclude every-day use at present. Whilst the present review's findings demonstrate a shift in focus towards strain analysis of internal soft tissue structures, it is likely that surface stress predictions and measurements will continue to be valuable. Clinically, they offer a more practical and lower cost socket assessment capability than invasive volume imaging techniques. In numerical modeling, experimental measurement modalities with higher spatial resolution and sensitivity will enhance validation, which is important to maintain confidence in model predictions as their sophistication and complexity increases.
Finally, some established imaging techniques have been applied more recently to amputated lower limbs and may provide additional input data for model tuning or validation. Alongside upright MR scanning, fluoroscopy has been used to measure relative displacement between the residual bone and socket under quasi-static loading [160], [161], simulated gait [162], and dynamic Roentgen stereophotogrammetric analysis has captured more strenuous activity [163].
6. Limitations
This review was conducted by engineers and health scientists only, so may demonstrate some interpretation bias. In an effort to prevent this, the main analysis was discussed with expert clinicians and other health scientists. The review also considered only publications in the English language literature, except for two cases where authors assisted with translation or interpretation.
7. Conclusion
Numerical modeling of the amputated limb has received less attention than many other musculoskeletal conditions, partially due to the smaller incidence of lower limb amputation than, for example, total joint replacement. However, the potential quality of life benefits of improving the comfort of the residual limb–prosthetic limb interface are substantial, for the life of the prosthetic limb user. From a purely mechanical perspective, however, the modeling complexity is high, featuring multi-body structures connected by contact pairs, highly nonlinear material models, and dynamic, variable loading conditions. Complicating matters further, inter- and intra-individual loading and anatomic variability are large, and influenced by surgical variability and prosthetic prescription. Extensive progress has been made in the interpretation of model predictions, considering thresholds for tissue injury and adverse adaptation. Other researchers have also attempted to include factors such as comfort and pain threshold, which are highly subjective and difficult to evaluate.
There is value in working towards highly accurate and detailed user-specific biomechanical models, but a key practical value in limb–prosthesis FE models is in contributing to evidence-based prosthetic limb fitting, and such a model's requirements would be rather different. Parametric models may enable comparative analysis of different prosthetic limb options, and the identification of potential risk factors, and worst cases for pre-clinical analysis of new technologies. Despite the described progress towards a clinically-translatable FE model automated user-specific socket design [38], these methods are still not in clinical use. Several considerations should be made for overcoming the barriers to clinical translation, which are common with all clinical decision-support tools. Experience of introducing IT systems in 1990s showed that the success of technology adoption is linked to the implementation management process and the receptiveness of clinicians [164]. This receptiveness, as well as the safety of the technology's use, are enhanced when technology is developed with end-user involvement [165]. Considering FEA in prosthetic limb fitting, collaboration with clinicians will enable the development of appropriate measurement methods to obtain model input data. Furthermore, appropriate design architecture may be developed, such that expert engineering input is not required [47]. Technically, simulations will require an optimal balance of computational expense and accuracy so that there is no assumption that high performance computing hardware or expensive commercial FEA software licences are procured by each clinic. As important, the use of a new clinical technology must not increase consultation time or cost, or impede the application of the users’ skill. This is essential in prosthetics and orthotics, where the clinical consultation is so personalized, and limb assessment through processes such as palpation are at the center of the clinician's application of their skill and experience.