1. Introduction
Bone shows the inherent capacity for regeneration as part of the repair process in response to injury and at the time of skeletal development or continuous remodeling throughout adult life. Bone regeneration is comprised of a well-organized series of biological process of bone induction and conduction, involving a number of cell types and intracellular and extracellular molecular signaling pathways, through a definite temporal and spatial sequence, in an effort for optimization of skeletal repair and restoration of skeletal function [1]. Bone formation depends on the cooperation of different aspects, such as: (i) specific cell types like mesenchymal stem cells (MSCs) and osteoclasts (ii) the scaffold (calcium hydroxyapatite, extracellular matrix molecules, etc.); (iii) expression of soluble molecules (cytokines, growth factors, hormones, ions, vitamins) and (iv) various mechanical stimuli [2], [3].
The signaling molecules can be categorized into three groups: (i) the pro-inflammatory cytokines, (ii) the TGF-β superfamily and other growth factors, and (iii) the angiogenic factors [4], [5]. Interleukin-1 (IL-1), Interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) have an imperative role in initiating the repair cascade. Cytokines also regulate the endochondral bone formation and remodeling. TNF-α promotes the recruitment of MSCs, induces apoptosis of hypertrophic chondrocytes at the time of endochondral ossification and offers osteoclastic function [6]. The TGF super-family includes BMPs 1–8, GDF-1, 5, 8, 10, TGF-β1, -β2, -β3 promote the various stages of intramembranous and endochondral bone ossification during fracture healing.
2. Bone morphogenetic protein – overview
BMPs are the most vital growth factors in bone formation and healing [6]. The osteoinductive capacity of demineralized bone matrix was discovered by Urist in 1965 [7]. Several types of BMP have been isolated through molecular cloning and recombinant BMP have been synthesized. BMPs are produced during fracture repair from mesenchymal cells, osteoblasts, and chondrocytes. Different BMPs work independently or in combination with each other and other members of the TGF super-family, to trigger a cascade of events that endorse the development of bone and cartilage [8].
BMP is a dimeric molecule consisting of two polypeptide chains held together by a single disulphide bond [9]. The alignment of amino acid sequences shows that a significant amino acid sequence identity exists among all the BMPs in the carboxy-terminal region of the protein [10]. Osteogenic protein-1 (OP-1) and BMP-2 crystal holds “hand shaped structure” consisting of two fingers of anti parallel beta strand and an alpha helical region at the heel of the palm [9]. Depending on the similarity of the primary amino acid sequences, BMPs are typically classified into four groups BMP2/4, BMP5/6/7/8a/8b, BMP9/10, and BMP12/13/14 [11].
These proteins have been segregated from different mammal bone such as mouse, rats, bovine, monkey, man and also from clonal osteogenic sarcoma lines. Extracted purified BMP showed satisfactory bone induction activity but it takes longer producing time, high cost and very less quantity. It was revealed that a microgram of BMP was present in a kilogram of bone. Wozney et al. [12]cloned and acquired the cDNA of BMP and expressed in eukaryocyte and prokaryocyte but the cost was too high and the quantity was not also high. BMP was isolated from osteosarcoma cells and gave an idea for vast extraction through long time in vitro culture [13]. A substantial amount of BMP was extracted from mouse Dunn osteosarcoma tissue using 4 M guanidine hydrochloride solution [14], [15]. Mizutani et al. [16] extracted BMP from bovine demineralized dentin matrix (DDM) and 3 mg of purified d-BMP was obtained from 100 g of DDM.
BMPs induces the formation of bone and cartilage in vivo. Various types of cells, including osteoblasts and chondroblasts, participate in the process of bone morphogenesis, and they are functionally regulated by BMPs [17]. They have multimodal action (i.e., chemotactic, metabolic, mitogenic, apoptotic effects, morphogenic, and their combination) depending on the concentration, exposure time and target cells [18], [19], [20].
3. Clinical application of BMPs
Till date number of clinical applications of BMPs are reported. The major application domains include spinal fusion, long bone fracture repair and oral and maxillofacial surgery. A brief review of each domain follows.
3.1. Spinal fusion
Spinal fusion using iliac crest bone graft may become a historical practice due to modern advances in bone morphogenetic proteins. Presently two specific BMPs (BMP-2 and BMP-7) with different carriers is being used to accomplish successful spinal fusion in pre-clinical and clinical studies [21]. Application of BMPs in spinal fusion and other fracture treatment has been summarized in Table 1. Kodera et al. [22] studied the effect of rhBMP-2 (recombinant human BMP-2) and ZA (Zoledronic acid) administered as a single systemic dose for spinal fusion and examined its feasibility for clinical application by using a rat spinal fusion model. This combination was efficient for increasing callus volume and reducing osteoclastic stimulation in spinal fusion although proper dose and an increase in fusion rate is unclear. Pelletier et al. [23] evaluated the lumbar spinal fusion using β-TCP (tri-calcium phosphate) granules and variable Escherichia coli-derived rhBMP-2 dose in sheep model. Their results confirmed improvement of new bone formation and fusion rate by using E-BMP-2 dose, while β-TCP alone was largely resorbed and did not attain fusion in the model at 12 weeks (Fig. 1).
Table 1. Application of growth factors on different subjects.
| Implant/carriers | Growth factor | Growth factor loading technique | Subject | Bone | Ref. |
|---|---|---|---|---|---|
| β-TCP | rhBMP-2 | Soaking (aqueous solution) duration: 15 min before implantation | Cross-bred ewes | Lumbar spinal fusion | [23] |
| HAp coated and uncoated Ti | BMP-2 | Soaking (aqueous solution) duration: not available | Labrador dogs | Femur | [27] |
| Collagen sponge | rhBMP-2 | Soaking (PBS) duration: just before implantation | Rat | Lumber spinal fusion | [28] |
| Gelatin hydrogel scaffold | rhBMP-2 | Soaking (PBS) duration: overnight | Rat | Lumber spinal fusion | [22] |
| Collagen sponge | Trapidil | Intraperitoneal injection | Mice | Calvarial bones | [29] |
| β-TCP | rhBMP-2 | Soaking (buffered solution) duration: over night | Beagle dogs | Long intercalated rib | [30] |
| Alginate hydrogel | rhBMP-2 | In-situ mixing before hydrogel preparation | Rat | Femur | [31] |
| Gelatin – βTCP sponge | BMP-2 | Soaking (saline) duration: 1 h | Horse | Splint bone | [32] |
| Particulate bone graft | BMP-2 | Infusion into zygomatic arch | Rat | Zygomatic arch | [33] |
| Bioactive glass | BMP-2 | Soaking (citric acid) duration: 24 h | Rat | Calvarial defect | [34] |
| Poly(propylene fumarate), PLGA | BMP-2 | Soaking (PBS) duration: 30 min | Rat | Femur | [35] |
| Demineralized bone matrix and collagen | BMP-2 | Not available | Rabbit | Mandible | [36] |
| Gelatin and bone flap | BMP-2 | Soaking (acetic acid) duration: not available | Monkey | Mandible | [37] |
| Bovine hydroxyapatite | BMP-7 | Not available | Human | Maxillary sinus | [38] |
| Natural non organic bone | BMP-4 | Gene therapy (mammalian plasmid vector expressing enhanced green fluorescent protein–human bone morphogenetic protein-4 (pEGFP-hBMP-4) was constructed through subcloning techniques) | Rabbit | Mandible | [39] |
| Collagen | BMP-2 | Soaking (medium: not available) duration: not available | Human | Spinal fusion | [26] |
| Collagen | BMP-2 | Soaking (aqueous solution) duration: 15 min | Human | Spinal fusion | [40] |
| Polyethylene glycol hydrogel | BMP-2 | Not available | Human | Transforaminal lumbar interbody fusion | [41] |
| Collagen | BMP-2 | Not available | Human | Lumber interbody fusion | [42] |
| Bone graft | BMP-2 | Not available | Human | Spinal fusion | [43] |
| Autologous bone graft | BMP-2/BMP-7 | BMP suspension was injected at nonunion site | Human | Forearm nonunion | [44] |
 Fig. 1. Micro-CT images of spinal fusion for different group after 12 weeks postoperatively [23]. The photograph shows that new bone formation and complete bone bridging in Group 1 and lower doses of BMP displayed comparatively less amount of new bone formation. Group 4 showed some amount of new bone formation and in Group 5 bone bridging was seen with delayed unions [image reproduced with the kind permission of Elsevier BV, North American Spine Society].
Fig. 1. Micro-CT images of spinal fusion for different group after 12 weeks postoperatively [23]. The photograph shows that new bone formation and complete bone bridging in Group 1 and lower doses of BMP displayed comparatively less amount of new bone formation. Group 4 showed some amount of new bone formation and in Group 5 bone bridging was seen with delayed unions [image reproduced with the kind permission of Elsevier BV, North American Spine Society].Autologous growth factor has been used on 39 patients having lumber spinal fusion [24] with no impending pseudo-arthroses on radiographic assessment at last follow-up visit. Solid fusion was confirmed in three patients having routine hardware removal and in two patients having surgery at an adjacent level. The effect of Autologous Growth Factors (AGF) was tested on lumbar inter body fusion through specific attention paid to find out clinical and radiographic outcomes [25]. In another study, a high-fusion rate was achieved with BMP-2 (low dose 1.4 mg) and local bone graft for minimally invasive lumbar inter-body fusion [26].
Till date, the uses of BMPs have been demonstrated clinically in only one level fusion. Spinal fusion often requires multiple levels especially in cases where deformity-correction surgery is required. The efficacy and use of BMPs in multiple levels with an appropriate carrier and dose has still not been established. Comprehensive understanding in this needed domain has been yet to develop. The major challenges of the future are to further optimize the dose and the carrier material for the specific fusion application, i.e. anteriorly, posteriorly, for repair of pseudarthrosis, multi level surgeries and instrumented cases.
3.2. Long bone fracture
BMPs are reported to play a pertinent role in the long bone fracture healing. They aid the repair of critical-sized segmental bone defects in animals by stimulating the migration of mesenchymal stem cells from periosteum, muscle, endosteum, and bone marrow into the defect via proliferation and differentiation of the mesenchymal stem cells, and by the formation of bone through endochondral ossification [45].
Various studies have been carried out to explore the effect of BMPs on healing of bone - defects. The effect of BMP-7 on allograft integration in a long-bone critical-size defect sheep model has been studied with faster callus formation and bone remodeling [46]. Azad et al. [47] evaluated the effect of BMP-2 in a diabetic rat segmental defect model and found improvement of new bone formation, higher mechanical stability and rapid consolidation than control. The repair of long intercalated rib defects has been studied using porous β- TCP cylinders containing rhBMP-2 in dogs [30]. By adding rhBMP-2 to the β-TCP cylinders, it promoted rib bone regeneration in the presence or absence of the periosteum. The alginate based hybrid system was used for growth factor delivery to repair the femoral defect in rat model [31]. It was observed that the nanofiber mesh tube with alginate without BMP did not show new bone formation, whereas after application of BMP new bone formation was achieved (as shown in Fig. 2).
 Fig. 2. Micro-CT analysis of bone regeneration at 4 and 12 weeks. The images illustrate that defects in Groups III and IV were filled with newly formed bone, while those in Groups I and II possessed limited new bone at the native bone ends and the defect periphery [31] [image reproduced with the kind permission of Pergamon, Biological Engineering Society].
Fig. 2. Micro-CT analysis of bone regeneration at 4 and 12 weeks. The images illustrate that defects in Groups III and IV were filled with newly formed bone, while those in Groups I and II possessed limited new bone at the native bone ends and the defect periphery [31] [image reproduced with the kind permission of Pergamon, Biological Engineering Society].The treatment of long bone defect is still a challenge. Though BMPs have strong osteoinductive effect, the standard therapies for critical sized defect are still distraction osteogenesis and autografting. With the improvement of biotechnology, larger bone defects can be treated with BMPs using synthetic carriers or graft materials and tissue engineering approaches.
3.3. Oral and maxillofacial surgeries
Bone grafts are often used to repair mandibular defects. Usually these defects occur due to traumatic injuries, surgeries for tumor removal or congenital defects. Bone grafts are also sometimes required to build a base for dental implant to strengthen and thicken dental sites. Studies evaluating the repair of mandibular bony defects using BMPs [37], [39], [48], [49] have shown that such an approach is effective in different animal models. The rhBMP-4 gene therapy combined with tissue engineering techniques was used to improve the repair of mandibular osseous defects in rabbits [39]. Zhou et al. [37] studied mandibular reconstruction with prefabricated tissue-engineered bone flaps and rhBMP-2 implanted in rhesus monkey. Homogeneous osteogenesis and bone regeneration was achieved using demineralized bone matrix (DBM) loading with collagen-targeting bone morphogenetic protein-2 [36]. Their studies suggested that the collagen-based BMP-2 targeting bone repair system induced better bone formation both in qualitatively and quantitatively as shown in Fig. 3.
 Fig. 3. Histological image of (1) DBM and (2) DBM with rhBMP-2, showing more amount of new bone formation using rhBMP-2 (NB = new bone) [36] [image reproduced with the kind permission of Pergamon, Biological Engineering Society].
Fig. 3. Histological image of (1) DBM and (2) DBM with rhBMP-2, showing more amount of new bone formation using rhBMP-2 (NB = new bone) [36] [image reproduced with the kind permission of Pergamon, Biological Engineering Society].In clinical setting, absorbable collagen sponge loaded with BMP-2 was applied for maxillary sinus floor augmentation [50]. Their study showed significant bone growth and overall mean height response for the maxillary sinus floor augmentation was 8.51 mm. The safety and effectiveness of rhBMP-2 on an absorbable collagen sponge (ACS) were compared with an autogenous bone graft on 160 patients when used for 2-stage maxillary sinus floor augmentation [51], [52]. Significant amount of new bone was formed by 6 months postoperatively with success rate of 79%. Till date, there are limited cases of clinical studies involving oral and maxillofacial surgeries using BMPs.
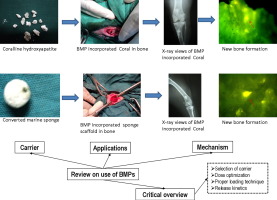
4. BMP delivery system
Carriers for BMPs are of paramount necessity to increase retention in the treatment area for an adequate period of time to permit regenerative tissue forming cells to migrate to the injured area and to proliferate and differentiate. These may also serve as a matrix for cell infiltration while retaining a space or volume in which repair tissue development can occur.
The essential requirements for ideal carriers for BMPs are listed below [6], [53], [54], [55]
-
•
Ability to incite the best possible inflammatory responses.
-
•
Construction of an interface with the adjacent biological tissue.
-
•
Ideal porosity in order to allow first the infiltration of cells and then vascular in-growth.
-
•
Adequate compressive and tensile strength.
-
•
Biodegradable but allow protection to BMPs from degradation for a period sufficient to stimulate a specific quantity of bone mass at the treatment area.
-
•
Non-toxic, sterile, immunologically inert and user-friendly.
-
•
Easy to manufacture (cost effective as well) for large-scale production.
-
•
Provision for continuous release of incorporated factors and release rate to be optimally controlled because of its short half-life in vivo.
5. BMP carriers
The retention of the BMPs in a delivery system may be performed by various methodologies by means of adsorption, entrapment or immobilization, or by covalent binding. The easiest way to deliver the growth factor is adsorbing rhBMPs to the surface of the implant, although the release of the protein may be less sustained. Furthermore, delivery of adsorbed growth factors often results in the initial burst release [6]. Immobilization of rhBMPs to implant surfaces usually showed a more sustained presence, but the protein cannot freely diffuse within the environment due to the covalent bonding. Entrapment and encapsulation of rhBMPs eliminates the issues of rapid release and immobilization and are the most accepted technique to deliver rhBMPs [55]. However, the difficulty arises over the fact that during processing of certain materials into carriers, pH conditions or temperature conditions often result in denaturation of the protein. Therefore, researchers were trying to develop specific methods to prepare the carrier system for BMPs which do not cause their loss of activity. There are three major categories of carrier materials like ceramics, synthetic polymer (PLA-PEG, PGA, PLGA, PLGA-PEG, etc.) and natural polymer (collagen, chitosan, silk fibroin, alginate, gelatin, etc.), ceramics (HAP, β-TCP, BCP). There are composite carrier materials as well. Some of the carrier materials used so far by different researchers are given in Table 2.
Table 2. Carrier materials for delivery of growth factor.
| Carriers | Subject | Growth factors | Loading technique of growth factor and media used | Ref. |
|---|---|---|---|---|
| Hydroxyapatite | Sheep | BMP-2 | Soaking (50% acetonitrile/0.1% trifluoroacetic acid) duration: not available | [56] |
| PLA/PGA copolymer and gelatin sponge | Rabbit | BMP-2 | Soaking (buffer consisting of 5 mmol l-glutamic acid, 2.5% glycine, 0.5% sucrose, and 0.01% Tween 80) duration: soaked before implantation | [57] |
| PLA-PGA copolymer and gelatin sponge (PGS) complex | Rabbit | BMP-2 | Soaking (buffer consisting of 5 mmol l-glutamic acid, 2.5% glycine, 0.5% sucrose, and 0.01% Tween 80) duration: soaked before implantation | [58] |
| Silk scaffold | Rat | BMP-2 | Soaking (buffer) duration: loading before implantation | [59] |
| Alginate hydrogel | Mice | VEGF and BMP-2 | In-situ loading | [60] |
| Alginate | Rats | BMP-2 | In-situ loading | [31] |
| Alginate | Mice | BMP-7 | Soaking (distilled water) duration: not available | [61] |
| Hydrogel of p(NiPAAm-co-AAc) copolymer and HAp | Mouse | BMP-2 | In-situ loading during hydrogel preparation | [62] |
| Acrylated hyaluronic acid | Rat | BMP-2 | In-situ loading during hydrogel preparation | [62] |
| Gelatin and β-TCP | Mice | BMP-2 | Soaking (aqueous solution) duration: overnight | [63] |
| Collagen | Mice | BMP-2 | In-situ loading into collagen gel | [64] |
| (poly-d,l-lactic-acid-para-dioxanone-PEG | Dog | BMP-2 | In-situ loading through polymer film fabrication | [65] |
| Gelatin poly(propylene fumarate) composite | Mice | BMP-2 | Diffusional loading (PBS) duration: 20 h | [66] |
| β-TCP | Dog | BMP-2 | Soaking (buffer of 5 mmol/l glutamic acid, 2.5 vol% glycine, 0.5 vol% sucrose and 0.01 vol% Tween 80) duration: few mins | [67] |
| PLA/PEG/HAp | Rabbit | BMP-2 | Soaking (buffer of 5 mM glutamic acid, 2.5% glycine, 0.5% sucrose, and 0.01% Tween 80) duration: not available | [68] |
| PLGA/Col | Mice | BMP-4 | Soaking (aqueous medium) duration: overnight | [69] |
| Chitosan | Mice | BMP-2 | Mixing | [70] |
| Chitosan-xerogel | Rat | BMP-2 | Soaking (PBS) duration: 3 h | [48] |
| Silk fibroin | Mice | BMP-7 | Soaking (SBF) duration: 1 week | [71] |
| Silk fibroin- polycaprolactone | Rat | BMP-2 | In-situ loading before gelation | [72] |
| Hyaluronan | Rabbit | IGF-1 | Mixing (IGF-1 in saline) | [73] |
| Hyaluronan/collagen | Rat | BMP-2 | In-situ loading during hydrogel formation | [74] |
| PCL/β-TCP | Sheep | BMP-7 | Soaking (saline) duration: not available | [75] |
5.1. Ceramics
Calcium phosphates are extensively used due to its osteoconductive properties and similarity in mineral composition, properties, and micro-architecture to human cancellous bone. But the materials are inherently brittle with very low fracture toughness and hence cannot be used in those cases where the component is subjected to high bending or tensile stress. Conversely, they have high bonding affinity for growth factors which makes them suitable for use in controlled delivery systems. Three categories of calcium phosphates are available e.g. calcium hydroxyapatite (HAp), Tri-calcium phosphate (TCP) and biphasic calcium phosphate (BCP). TCP-HAp composite material exhibited a very high affinity for rhBMP-2. The rhBMP-2/ceramic interaction depends on hydroxyl, amine and carboxyl groups in BMP-2 [76], [77] and on the number of divalent ions Ca2 + present in the ceramic. Calcium phosphate coatings are reported to incorporate growth factors into the lattice-work of mineral layers. BMP is also biomimetically deposited during the formation of calcium phosphate film. Apart from calcium phosphates, bioglass microspheres has also shown promising potential as carrier material because of its osteoinductive nature. Perez et al. used silica based bioactive glass for delivery of fibroblast growth factor and showed that it was capable to sustainably deliver therapeutic molecules [78]. Calcium phosphate cement based 3-D printed scaffold also used as delivery system of growth factor and other biomolecules [79].
5.2. Synthetic polymers
There are large numbers of synthetic polymers that have been used in tissue engineering application for their degradability, biocompatibilities, formability and ease of use. The synthetic polymer can be specifically modified by simple processing for the desirable physical, chemical and mechanical properties. For BMP delivery PCL, PEG, PLGA are extensively used. These synthetic materials are combined with other osteoconductive materials like HAP, TCP etc. for delivery of BMPs.
PLA/PEG/HAp composite served as good carrier for BMP-2 and it showed repair of articular cartilage defect within three weeks in rabbit model [80] and repair of radius bone defect in rabbit within eight weeks [68]. Poly d,l-lactic acid-p-dioxanone-polyethylene glycol block copolymer (PLA-DX-PEG) combined with β-TCP and low dose of BMP-2 resulted in putty like material formation having superior handling, fabrication and osteoinductive properties. The composite material showed good response in vivo study using low dose of BMP-2 [81]. Slow release system of PEG hydrogel has been assessed for glycosylated and nonglycosylated rhBMP-2 delivery. It is shown that PEG hydrogel interacted less with glycosylated rhBMP-2 and have more bioactivity as compared to non-glycosylated rhBMP-2 [82]. Because of the strong affinity of deproteinized bovine bone matrix (DBBM) and rhBMP-2, PEG hydrogel could be a potential carrier system for rhBMP-2 delivery.
PLGA/collagen hybrid scaffold had osteoinductive activity to human MSCs with long stimulation effect over a period of four weeks in vivo [69]. Chitosan/PLGA composite scaffold showed controlled release and improved bioactivity of BMP-2 in vitro [83]. PLGA copolymer with RADA16-P24 peptide is capable of attaching bone MSCs in vitro and induced ectopic bone formation in vivo [84]. PLGA and calcium phosphate composite microparticles loaded with BMP and VEGF showed enhanced osteogenesis and angiogenesis in vitro. The microparticles had high encapsulation efficiency of BMP and VEGF. In vivo results showed good biocompatibility, osteogenic and angiogenic activity [85].
Polycaprolactone (PCL) is another accepted, commercially accessible polymer used in tissue engineering applications for its solubility in many organic solvents and it can form miscible blends with numerous polymers and is hydrolytically degradable (2–3 years). Cell culture assessment showed that scaffold allows proliferation and differentiation of fibroblasts and osteoblasts PCL-TCP scaffolds seeded only with canine osteoblasts could sustain excellent osteogenic expression in vitro [86]. Injectable nanofibrous scaffold by incorporating PCL into collagen matrix could provide controlled release of BMP-2 for three weeks without loss of its bioactivity and showed osteoblastic differentiation in in-vitro culture [87]. It was proved as a suitable biomechanical and biochemical environment to act as a reservoir for osteogenic factors with controlled release profile. In another study, BMP-2 immobilized PCL fibers modified with heparin-dopamine (Hep/PCL) induced osteogenic differentiation of periodontal ligament cells [88]. The Hep/PCL fibers showed sustained BMP-2 release profiles over 28 days and significantly induced osteogenic differentiation of PDLCs with a significant increase in ALP activity and calcium deposition. PCL and β-TCP composite scaffold showed bone regeneration in critical size defect in sheep using low dose of BMP-7 [75]. The binding affinity and release of growth factors of PCL nanofibers can be modified using mineral coatings. VEGF and BMP-2 were bound with efficiencies up to 90% to mineral mineral-coated PCL scaffolds [89].
3D printed Polymer hybrid materials can be used as biomedical scaffolds for regenerative medicine. There is tremendous scope for supramolecular materials and their composites in 3D printing of complex structures. [90]. Synthetic and biodegradable polymer-inorganic composite are very promising as tissue engineering scaffold. The advantages of these type of scaffolds includes its machinability, bioactivity and controlled degradation kinetics. The inorganic bioactive phases were incorporated to porous interconnected 3D polymer networks [91]. Organic-inorganic hybrid scaffold were also developed in tissue engineering application. 3-(Trimethoxysilyl)propyl methacrylate and octafunctionalized cage-like polyhedral oligomeric silsesquioxane hybrid scaffold is a potential device for delivery of biomolecules [92].
5.3. Natural polymers
Collagen is marked as ‘gold standard’ as a delivery system for BMPs. Collagen is the most abundant protein available in mammals and it provides the structural matrix for tissue regeneration. It can be used as films, gels and sponges and also ideal for bone defect treatments due to its high binding affinity to BMPs and its osteoconductive properties. It is biocompatible and advantageous for cell adhesion, proliferation and cell differentiation. FDA approved two models collagen sponges to deliver BMP-2 and BMP-7 for spinal fusion and long bone fracture. Collagen membrane can be used for sequential delivery of BMP-2 and BMP-7 for bone regeneration in vivo [93]. Collagen-1 combined with BMP-2 synergistically improved the osteogenesis of MSC [94]. The major disadvantages are sourcing, processing, probable disease transmission and immunogenicity [48] including lack of mechanical strength and unpredictable biodegradability of the collagen matrix.
Chitosan is effective for promoting bone mineralization and cell activation. It is a promising new source for scaffold material for tissue regeneration due to its potential for functionalization, conductive and inductive nature. Chitosan is obtained by alkaline deacetylation of chitin, derived from exoskeletons of arthropods. Chitosan has inherent capacity to bind and retain proteins in biologically active manner. Several studies have been reported the use of chitosan composite for delivery of BMPs. Lee et al. [80] used hybrid of chitosan-xerogel membrane for delivery of BMP-2 to evaluate its effect in vitro and in vivo. The in vivo study demonstrated that the bone regeneration is significantly higher using the hybrid carrier compared to control. Chitosan- ammonium hydrogen phosphate (AHP) composite was also reported to encapsulate rhBMP-2 in a bioactive form indicated by the improvement of ALP activity of osteoblast cells in vitro and ectopic bone formation in vivo [95]. To get prolonged release of BMP from chitosan carrier, chemical modification was reported to make it negatively charged [70]. The group showed that low dose of sulfated chitosan stimulated osteoblast differentiation and promoted ectopic bone formation in vivo.
Silk fibroin (SF) is a potential biomaterial for its unique structural properties, self-assembling ability, mechanical strength, processing flexibility, biodegradability, and biocompatibility. SF is extracted from cocoons made by larvae of silk worms. It is available in various forms like membrane, mesh, fiber, film, sponge etc. it is extensively used as a platform for drug delivery as film and silk elastin hydrogel form. BMP-2 can be directly immobilized on silk using carbodiimide chemistry. Silk fibroin provides sustained release of IGF-1 [96]. Positively charged IGF-1 creates ionic bonds with negatively charged silk fibroin. The researchers showed the modification of SF under mild condition to sustain its activity. Zhang et al. [71] tested SF as BMP-7 carrier which showed sustained release for 21 days and support cell proliferation and differentiation. New bone formation was achieved when tested in-vivo in a critical size calvarial defect in mice. Surface modification of SF by plasma irradiation method induced new bone formation when tested in femur critical size defect in rabbit [97]. Electrospun polycaprolactone (PCL) nanofiber mesh tube with a silk fibroin hydrogel is also a promising carrier for delivery of BMP-2 for the treatment of large bone defect [72].
Alginate is a water soluble anionic and hydrophilic polysaccharide extracted from brown seaweed and bacteria. It is widely used as supporting matrix or delivery system for tissue repair and regeneration. The property of alginate material includes biocompatibility, biodegradability, chelating ability and non-antigenicity. Alginate exhibits a pH dependent anionic nature and it interacts with the cationic polyelectrolytes and proteoglycans. Divalent cation alginate crosslinked with BMP-7 by covalent bonding and showed retention of growth factors and sustain release [61]. In-vivo study suggested that alginate is highly effective carrier for BMP having bone forming effect. Alginate-PLGA composite microparticles performed as carrier when it implanted in rat [98]. An alginate based system containing rhBMP-2 in nanofiber mesh showed sustained spatiotemporal release, which is effective in the repair of critical-sized segmental bone defects in a rat model [31].
Gelatin is commercially available derived from collagen that is generally crosslinked or hardened through thermal treatment to reduce its high water solubility and enhance the retention of protein to get long term release. BMP-2 loaded into gelatin sponge is effective for in-vivo osteoinduction when it was implanted subcutaneously into middle aged mice [99]. Gelatin/β-TCP sponge incorporated BMP-2 had therapeutic effect for the treatment of metacarpal bone defect in horse [100]. Gelatin/β-TCP sponge showed release of BMP for 28 days in-vivo. Homogeneous bone formation was observed throughout the sponges when applied in mice [63] and in rabbit [101]. Gelatin electrospun fiber is a promising scaffold for bone tissue engineering. Gelatin scaffold is a good carrier for controlled release of BMP-2 which induced osteo-differentiation of MSCs [102]. BMP-2 released from gelatin microparticles exhibited minimal burst release followed by sustained release in-vitro. The systematic control of BMP-2 delivery from gelatin MPs can be achieved in-vitro and in-vivo by altering the extent of basic gelatin crosslinking [66].
Hyaluronan (HA) is fully biocompatible, non-immunogenic and readily available in medical grade. HA is a natural component of extra cellumar matrix (ECM) playing a key role tissue repair. HA improve the osteoconductive property of calcium phosphate [103]. HA-TCP composite is able to provide controlled release of BMP-2. HA inhibits BMP induced osteoblast differentiation through CD44 receptor [104]. Hyaluronan is proved as effective carrier for intra-articular injection of IGF-1 and it have positive role for cartilage and sub-chondral cancellous bone repair in temporomandibular joint in rabbit [73]. HA control the burst release of BMP from collagen matrix and HA/Col composite prove sustained release which is desirable for bone formation [74].
5.4. Microparticles and nanoparticles
Microparticle (MP) and nanoparticle (NP) based delivery system have been extensively used for localized delivery and sustained release of growth factors. Commonly used materials for the design of nanodevices includes natural polymers, synthetic polymer and calcium phosphate based particles. Microparticles are small free flowing particles consisting of natural or synthetic polymers having particle diameter ranging from 1 to 1000 μm. PLGA based delivery system have been extensively used for BMPs delivery. PLGA MPs carriers allow the stability and controlled delivery of BMP. Quinlan and coworker used alginate and PLGA MPs as rhBMP-2 carriers and assessed the effect of incorporation of different amount of polymer into porous HAp-collagen scaffold for bone regeneration [98]. The in vivo study on rat model showed new bone formation. The result also proved the beneficial role of PLGA as growth factor carrier due to its protecting ability from degradation in vivo. Bratt-Leal et al. [105] presented gelatin based MPs which can serve as a delivery system for BMPs. The group showed that gelatin MPs loaded with BMP-4 and noggin induced efficient gene expression of mesoderm and ectoderm lineages without affecting the loss of pluripotency. Microparticles based growth factor delivery system is an attractive alternative for efficiently scale-up production of differentiated cells from embryonic stem cells. In another study, Glycosaminoglycans (GAGs) based material heparin MPs was used for binding and retention of growth factors [106]. Heparin MPs has ability to bond considerable amount of growth factors like BMP-2, VEGF and FGF-2 and < 25% of bound growth factors were released over a period of 28 days.
Nanoparticles are solid, colloidal particles that comprised macromolecular substances. The nanoparticle drug delivery system is advantageous due to its nanometer size (10–1000 nm) and higher surface to volume ratio. It also provides reduced protein diffusion and retains sufficient concentration for recruitment and differentiation of osteoprogenitor cells. Polymeric nanoparticles prepared from natural and synthetic polymers are popular for its stability and ease of surface modification. They can be tailor-made to attain both controlled drug release and disease-specific localization by alteration of the polymer characteristics and surface chemistry. Mercado et al. [107]developed biodegradable NPs from succinimide-terminated poly(lactide fumarate) (PLAF-NHS) and poly(lactide-co-glycolide fumarate) (PLGF-NHS) macromers. Another biodegradable polymer NPs using catechol-poly(l-aspartic acid)-b-poly(l-phenylalanine) (Cat-PAsp-PPhe) was developed by Lee et al. [108] for controlled release of BMP-2. Dual interacting polymeric nanoparticle (D-NP) was prepared by Seo and coworkers using thermo sensitive poly (phosphazene) [109]. The D-NP formed nanocomplex with BMP-2. The ionic and hydrophobic interaction of D-NP/BMP-2 nanocomplex showed a synergistic effect on sustained BMP-2 release for a period of three weeks in vitro. The group reported higher osteocalcin secretion in C2C12 cells and significant bone generations by the BMP-2 exposure.
All the carriers discussed so far may or may not require functional groups depending on the desired loading and release kinetics of growth factors. The process of functionalization requires proper optimization that demands a thorough and detailed study on the chemistry and related characteristics of the carrier-BMP interface (Table 3).
Table 3. Microparticles (MP) and nanoparticles (NP) for growth factor delivery system.