1. Introduction
The common model of therapy known as ‘one-size-fits-all’ has resulted in moderate success for the predominant group of patients. Despite the fact that an appropriate drug is taken at an appropriate dose and in an appropriate manner, numerous side effects are often reported [1]. A vast amount of adverse drug reactions is due to overdosing because individual variability does not comply with the manufacturer's recommended dosages [2]. A modern therapy allowing one to apply for a single patient the best suited drug which needs to be delivered in the right place and at the right time could be a solution to reduce adverse effects, accelerate patient recovery, and finally ensure positive therapeutic effects [3].
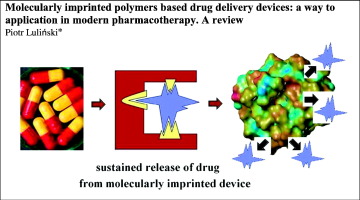
The traditional pharmaceutical formulations commonly did not fulfill the demands of modern pharmacotherapy. Thus, extensive studies were carried out to develop new drug delivery devices suitable for such a purpose [4], [5], [6]. The above efforts were facilitated by great progress in technology and material science, for instance novel nanobiomaterials such as polymeric nanofibres for drug delivery or liposomes for gene delivery. These materials offer improved transport properties, provide optimized pharmacokinetic profiles, control the drug release rate and maintain the drug concentration within its therapeutic window as well as enhance delivery efficacy by increasing diffusivity and biodistribution. However, the commercial application of novel drug delivery materials still poses a great challenge for modern pharmacotherapy. The optimum drug delivery carrier should be synchronized with the physiological status of the patient and should provide a drug in response to the changing intracorporeal environment [7]. Here, the molecularly imprinted polymers (MIPs) could be a group of materials that have great potential in the drug delivery for modern pharmacotherapy.
Molecularly imprinted polymers are promising materials in the construction of drug delivery devices because they can provide improved delivery profiles and longer release time as well as extended residency of the drug [8], [9]. This class of polymers could also release the drugs in the feedback regulated way, which could be extremely important in a modern model of pharmacotherapy oriented towards the delivery of the best suited drug to a single patient in the right place and at the right time. Finally, MIPs are highly selective materials capable of maximizing the delivery of a given eutomer, the isomer of interest, and of reducing or even eliminating the delivery of the distomer, the undesirable isomer [10], [11].
In spite of its great potential, the application of MIPs in drug delivery is still at the developing stage. In recent years we could observe significant progress in the synthesis of MIPs for drug delivery with novel sophisticated formats of polymers. However, this progress does not correspond to the implementation of MIPs in modern pharmacotherapy. Thus, a question arises why such promising materials cannot find a widespread applicative role in the field of drug delivery?
In this review, different barriers that prevent the implementation of MIPs into pharmacotherapy will be outlined in order to formulate the answer to the above questions. First a brief overview of the imprinting process together with a concise description of drug release mechanisms from the imprinted materials will be presented. Then the present status of MIPs as potential drug delivery devices for ocular, transdermal, intravenous and oral routes of administration will be discussed with emphasis on biocompatibility, cytotoxicity, and in vitro or in vivo behavior of MIPs. Current barriers that prevent implementation of MIPs into pharmacotherapy will be identified. Finally, future prospects for imprinted drug delivery forms will be outlined.
2. Insight into imprinting process
The molecularly imprinted polymers are characterized by a high level of selectivity due to the presence of specific recognition sites formed in the polymer network by the template-tailored synthesis. The synthesis of imprinted materials consists of the following steps: the formation of the prepolymerization structure, the polymerization reaction and the template removal (Fig. 1). The formation of the prepolymerization structure could be obtained by covalent or non-covalent strategies. The covalent approach assumes that there is a chemical reaction between the template molecule and the functional monomer that is necessary in order to form a functionalized compound prior to the polymerization. The non-covalent approach utilizes a range of weak intermolecular interactions such as ionic forces, hydrogen bonds, or π-π interactions that can exist between the template molecule and the functional monomer. The various aspects of the imprinting process were accurately described in numerous reviews and book chapters [12], [13].
 Fig. 1. A schematic presentation of the imprinting process.
Fig. 1. A schematic presentation of the imprinting process.The main parameter describing the efficacy of the imprinting process is called the imprinting factor. In simple terms, the imprinting factor is defined as a ratio of the binding capacity of the template on the imprinted polymer to the binding capacity of the template on the non-imprinted reference polymer. Hence, the synthesis of the non-imprinted polymer has to be carried out in the same conditions omitting the addition of the template molecule.
The specificity of imprinted polymers could be affected by formats of material. Depending on the synthetic strategy various formats of MIPs can be obtained. Let me mention here some of the formats that were recently designed and investigated as potential drug delivery devices: molecularly imprinted soft contact lenses and bioinspired metal ion coordinated hydrogels [14], [15], imprinted transdermal patches [16], imprinted like biopolymeric micelles [17], imprinted magnetic nanoparticles [18], [19], [20], composite hydrogel delivery systems [21], molecularly imprinted layer-coated hollow polysaccharidemicrocapsules [22], biodegradable imprinted drug delivery nanostructures [23], [24] and others [25], [26]. Those formats of MIPs were evaluated for the following routes of drug administration: ocular, dermal, intravenous and oral with extended support of in vitro and in vivo analyses of drug release as well as cytotoxicity tests. The above examples will be discussed in the next sections of this paper to outline the current barriers as well as to present the ways to overcome the problems in both synthetic and biological aspects. But first, a brief overview of the possible release mechanisms from imprinted materials will be presented in order to emphasize the advantages of MIPs as drug delivery carriers.
3. Drug release from imprinted devices
The determination of drug release kinetics from the imprinted polymers is very important considering their application as the drug carriers. In general, the nature of the imprinted matrix plays a crucial role in release of a drug. Here, the swelling controlled systems such as low cross-linked hydrogels or non-swelling controlled systems such as more rigid polymer networks could be considered. In the latter systems, the relaxation of the polymer matrix governs the penetration of physiological fluid inside the net and the transport is characterized by Fick's laws of diffusion [27].
However, in various imprinted systems the anomalous transport mechanisms are observed. In the imprinted materials, numerous complementary or sterically oriented functional residues interact with the drug delaying its release despite the swelling degree of the polymer. The strength of those interactions can be responsible for a sustained release. The delayed release can also be explained by the so-called tumbling effect which is described as the migration of the drug from one binding (imprinting) site to another. Thus, the release of a drug occurs due to multiple interactions of the drug through the network imprinted by it. The drug moves from one imprinting site (specific macromolecular memory site) to another where the complexation takes place and then it escapes from it and moves to another one. This behavior is responsible for longer mean residence time of the drug in the net [28]. In another imprinted system, the competitive binding of a compound that is present in the intracorporeal environment can be a factor which promotes the release of the drug embedded in the specific site of the imprinted device [29]. Those imprinting systems are extremely interesting as drug carriers because they can respond to the changes of concentration of an important bioanalyte or a biomarker. Finally, there is also a mechanism that involves the release of a drug in the physical stimuli-responsive manner, for instance as a consequence of response to a shift of pH of external fluids [22].
4. Current status of imprinted formulations
In this part of the review the current status of molecularly imprinted drug delivery devices will be presented pointing out the barriers that prevent the implementation of MIPs in modern therapy. The problems will be discussed with respect to obstacles resulting from the nature of the imprinted material as well as barriers of any particular route of drug administration to which the imprinted drug delivery device was designed, viz. ocular, dermal, intravenous and oral.
4.1. Imprinted soft contact lenses for ocular route of administration
The available ocular pharmaceutical formulations such as eye drops are characterized by low effectiveness of ophthalmic drug delivery. The protective mechanisms of the lacrimal apparatus and fast removal of drugs from anterior segments of the eye by the nasolacrimal drainage are responsible for low bioavailability. The application of ophthalmic ointments and gels only slightly improves the therapeutic effects. The bioavailability of ophthalmic drugs significantly increased when the ophthalmic contact lenses drug delivery systems were introduced into the treatment. However, low loading capacity and insufficient control over the drug release profiles from such devices are considered to be the main limitations [30].
Molecularly imprinted hydrogels were extensively investigated as the ocular drug delivery forms hoping to overcome the existing problems and to find a suitable delivery device for the treatment of glaucoma, one of serious progressive diseases related to the damage of optic nerves which can cause blindness as well as to provide non-steroidal anti-inflammatory drugs into the conjunctival sac. The model molecules of S-timolol (non-selective β-adrenergetic receptor antagonist) and acetazolamide (carbonic anhydrase inhibitor) as well as R/S-flurbiprofen, ibuprofen or diclofenac were selected as target drugs for which the imprinted devices were designed.
The molecule of timolol possesses chiral carbon atom and only the Senantiomer has high pharmacological activity. Thus, the design of drug delivery form to deliver the necessary eutomer is a major scientific challenge. In systematic studies various synthetic parameters were optimized to fabricate soft contact lenses based on imprinted hydrogel [9], [31], [32], [33]. The imprinted soft contact lenses were obtained by co-polymerization of methacrylic acid (functional monomer), N,N-diethylacrylamide (backbone monomer as well as solvent), and ethylene glycol dimethacrylate (a cross-linker at various concentrations) in the presence of S-timolol (template). The polymerization was carried out in mould that finally forms contact lenses with a diameter of 16 mm and thickness from 0.3 to 0.08 mm which corresponds to the greatest thickness of commercially available contact lenses. The thickness of the device is a very important parameter because it affected the release profile due to the length of the diffusional path through the hydrogel network [34]. First, the template removal step was carried out and total discharge of the template was ensured because the leaching of the template (or the so-called bleeding effect) is an undesirable consequence of the use of template in the prepolymerization mixture as well as unacceptable when the material is considered as a drug vehicle [35].
The adsorption (drug loading) of the target S-timolol was carried out using the soaking procedure. The binding capacities of imprinted hydrogels were determined revealing two times higher adsorption capacity of the imprinted material than of the non-imprinted one. The dissociation constants were between 5.0 and 8.9 μmol L− 1 (depending on the concentration of a cross-linker) for the imprinted hydrogels and between 6.3 and 29.4 μmol L− 1 for the non-imprinted ones. The in vitro release experiments were carried out in a 0.9% sodium chloride aqueous medium imitating the physiological conditions of the ocular surface. The release profiles of S-timolol were analyzed. The Higuchi model was employed for the analysis of drug release kinetics revealing that the transport of a drug from imprinted hydrogel was characterized by Fick's laws of diffusion. However, the presence of physiological saline strongly affected the diffusion of a drug and the release process. The in vivo experiments of S-timolol release from the imprinted contact lenses inserted in rabbit cornea were also carried out [33]. S-Timolol was detected in the tear fluid for a period of 180 min, which was two times longer than that from the non-imprinted hydrogel. A comparative analysis of S-timolol released from the eye drops containing 0.068% and 0.25% of S-timolol showed the presence of the drug in the tear fluid for only 60 min. It was also found that the ocular bioavailability of S-timolol from the eye drops only slightly depended on the dose, but the corresponding bioavailability from the presoaked imprinted soft contact lenses increased significantly (for 34 μg of timolol the AUC – area under curve values were 1.24 and 10.76 mmol min− 1 L− 1, respectively). Thereby, the physiological environment of the eye together with continuous renovation of the lacrimal fluid and the blinking affected the release behavior of S-timolol from imprinted soft contact lenses and decreased the ability of the device to a sustained release. Moreover, the release patterns from both imprinted and non-imprinted hydrogels were similar. This finding could be explained by insufficient specificity of the imprinted cavity.
Taking into account the fact that the imprinting process within the hydrogel network is explained by macromolecular memory of the template, only the regions with sufficiently high affinity can enable the increase of imprinted hydrogel binding capacity and improve the sustained release profile from the imprinted device [36]. Thus, in order to improve the specificity of imprinted hydrogels, the bioinspired imprinted hydrogel for ocular route of administration of carbonic anhydrase inhibitors was constructed [14]. The imprinted cavity in hydrogel network was designed to imitate the cone shape of the active site of human carbonic anhydrase II enzyme. Here, the components of the prepolymerization mixture involved 2-hydroxyethyl methacrylate (backbone monomer), 4-vinylimidazole, N-hydroxyethyl acrylamide and zinc(II) methacrylate (functional monomers) and acetazolamide (template). The functional monomer containing zinc(II) ions was used because in the active site of the enzyme, the zinc(II) ions interact with three histidine residues. After the synthesis, the affinity of hydrogels towards acetazolamide (template and the targeted drug) and ethoxzolamide (another drug, a structural analog of acetazolamide) as well as the release behavior of both compounds were analyzed. The binding capacities obtained for acetazolamide and ethoxzolamide were 3.28 to 1.71 mg g− 1, respectively. These results highlight the benefit derived from imitating the architecture of a physiological receptor for the design of the imprinted material. However, the acetazolamide and ethoxzolamide release data fitted into the Higuchi model revealing a sustained release of the latter drug. In the interpretation of the above results certain factors such as the solubility of a drug in releasing the medium and the network/water participation coefficient have to be considered. In order to ensure the biocompatibility of novel material the cytotoxicity studies were carried out on Balb/3T3 clone A31 cell line. Fibroblast showed excellent viability indicating that the hydrogel matrix consisting of the above components does not reduce the cytocompatibility and that there is no leakage of toxic compounds from the network. However, the imprinted hydrogels were slightly opalescent because of the presence of zinc(II) methacrylate. This phenomenon could be a problem for contact lenses. Moreover, the oxygen permeability was lowered because of the presence of residues from 4-vinylimidazole in the matrix. Insufficient oxygen permeability is a major barrier for wearing monthly soft contact lenses.
Therefore, the nature of monomers on the drug release profiles was investigated and 3-[tris(trimethylsiloxy)silyl]propyl methacrylate was selected as the functional monomer for analysis [31]. This monomer provides hydrogel with very good oxygen permeability and is often used as a component of wearing monthly soft contact lenses. The imprinted hydrogel matrix was built up from 3-[tris(trimethylsiloxy)silyl]propyl methacrylate as well as methacrylic acid (both used as functional monomers), N,N-diethylacrylamide (backbone monomer) and ethylene glycol dimethacrylate (a cross-linker) in the presence of S-timolol (template). The diffusion coefficient obtained for imprinted hydrogel based on 3-[tris(trimethylsiloxy)silyl]propyl methacrylate confirmed that S-timolol was released in a sustained mode as compared with the imprinted hydrogel based on 2-hydroxyethyl methacrylate backbone with the following values: 71.3 × 10− 9 to 9.9 × 10− 9 cm2 s− 1, respectively. Thus, by modulating the hydrogel composition it was possible to adapt the drug release behavior for imprinted soft contact lenses with better oxygen permeability.
In order to obtain imprinted soft contact lenses without any discoloration as well as with higher binding capacity of the device, an innovative method using a supercritical fluid technology was employed [37], [38]. This method used hydrogel based commercial soft contact lenses, viz. Hilafilcon B®. Subsequent impregnation imprinting and desorption steps were performed with the non-steroidal anti-inflammatory drug R/S-flurbiprofen as the template using the supercritical carbon dioxide technology. The rearrangement of polymeric regions of soft contact lenses in the presence of the template as well as the effect of supercritical carbon dioxide on the plasticization of hydrogel was responsible for the imprinting effect. Here, each consequent impregnation step resulted in an increase of binding capacity of the imprinted soft contact lenses. The release profiles were investigated. The release of R/S-flurbiprofen was sustained for 6 h in an aqueous medium. In another example, the supercritical carbon dioxide was used to fabricate S-ibuprofen soft contact lenses [39]. The imprinted hydrogel was built up only from 2-(dimethylamino)ethyl methacrylate (functional as well as backbone monomer) and ethylene glycol dimethacrylate (a cross-linker) in the presence of S-ibuprofen (template). The in vitro release behavior showed a strong dependence on pH of the releasing medium. At neutral pH anomalous transport was observed and the release of S-ibuprofen after 24 h was equal to 181 mg g− 1 for the imprinted hydrogel and only 65 mg g− 1 for the non-imprinted one. At acidic pH the release was close to zero order kinetics according to the Korsmeyer-Peppas model which was employed for the analysis of the drug release profile. The zero order release kinetics is strongly encouraged because it allows one to deliver the drug in a controllable manner.
In another valuable paper related to the evaluation of release kinetics from the imprinted material, the analysis of daily disposable imprinted contact lenses for delivery of diclofenac was presented [40]. This analysis revealed the effect of certain variables such as the correct volume or adequate exchange of the release medium on the evaluation of drug release kinetics from contact lenses. The commonly applied drug-eluting lens models involve small volumes of the poorly mixed release medium. Such a model assumed that the concentration of the drug in close proximity to contact lenses is negligible. In most cases, it revealed that the drug release is characterized by Fick's law of diffusion. Here, the imprinted polymer matrix of poly(2-hydroxyethyl methacrylate-co-N,N-diethylaminoethyl methacrylate-co-polyethylene glycol dimethacrylate) was selected as the most suitable network for a controlled release of diclofenac. The imprinted soft contact lenses had a base curve of 8.6 mm and a diameter of 15 mm with center thickness of 105 μm. The dimension and thickness were similar to commercial lenses. The release experiments were carried out in the microfluid chip device where a drug loaded imprinted soft contact lens was placed in a chamber and a releasing medium was capable of flowing across it. This model allows one to imitate the physiological ocular flow. It was demonstrated that under physiological flow conditions mimicking those in the human eye, the concentration gradient is the main driving force for the release of diclofenac. Here, the constant release rate of 8.74 μg h− 1 of diclofenac for the first day was observed which corresponds to 28% of the total amount of the drug loaded. For the next six days the release of 78% of diclofenac loaded was noted. Thus, the slow constant release of diclofenac from imprinted daily disposable lenses was achieved revealing close to zero order kinetics (diffusion exponent n = 0.935, when n is equal to one, the time independent release is performed). The release of diclofenac in a typical model was also carried out for comparison showing a release of 52.50 μg h− 1 of diclofenac for the first day and complete release within three days. Thus, the choice of the appropriate model for release experiments could play a crucial role in prediction of drug release behavior from imprinted soft contact lenses.
Summing up, extensive studies towards fabrication of novel imprinted soft contact lenses for drug delivery to ocular administration were carried out also for other therapeutic agents [41], [42], [43], [44], [45]. The physico-chemical parameters of imprinted ocular devices were improved and appropriate models for release analysis were proposed. Nevertheless, the lack of systematic in vivorelease experiments constrains their practical application in modern therapy.
4.2. Imprinted materials for dermal delivery
Skin is widely used as a route of administration for local and systemic drugs. The dermal route could also be an alternative for oral drugs which are characterized by low adsorption from the gastrointestinal tract or extensive first-pass metabolism of the drug. However, the problems that often occur on the surface of the skin can be a barrier for selected drugs. On the other hand, the compounds that can penetrate the skin surface easily are characterized by facile penetration of the polymer matrix, which makes it difficult to control their release rate from the device. Advanced investigations were carried out to introduce an efficient transdermal delivery of nicotine as well as propranolol in order to enhance their therapeutic effects [46]. Here, the imprinted materials with specific release mechanisms can be a solution.
In one useful paper, the molecularly imprinted nicotine transdermal system was proposed [16]. This imprinted system based on the copolymer of methacrylic acid and ethylene glycol dimethacrylate was polymerized by the bulk technique in the presence of nicotine as the template. The bulk imprinted material was crushed as well as ground and the particles of 75–106 μm were dispersed in mineral oil or propylene glycol prior to packing onto an aluminium foil disk of a surface equal to 1.8 cm2. The pH of the nicotine imprinted delivery system was similar to pH of the skin. For comparison, the commercial patch Nicopatch® (14 mg/24 h) was also analyzed. Here, the skin permeation studies were performed across porcine ear skin. The in vitro experiments revealed that the amounts of nicotine that permeated from the imprinted transdermal system and commercial patches were similar and equal to, respectively, 655 and 709 μg cm− 2 for 24 h. The experiments disclosed a strong impact of the polarity of the vehicle on the release of nicotine from the imprinted transdermal system. Finally, a few limitations of the imprinted nicotine system can be identified. Firstly, the use of organic components for fabrication of the imprinted polymer network could be the source of undesirable skin hypersensitivity. Secondly, the high burst effect that was observed during in vitro experiments can lead to an uncontrolled increase of nicotine levels in the circulatory system.
In order to improve biocompatibility of the imprinted transdermal system, the imprinted membrane for the stereoselective delivery of S-propranolol was proposed [47]. The membrane was a composite of the imprinted polymer integrated with cellulose which allows one to overcome the skin allergic reactions related to the application of organic components of the material. The cellulose membrane is a biocompatible and biodegradable material with good mechanical properties. The surface of the cellulose membrane was modified with a thin layer of R-propranolol or S-propranolol imprinted copolymer additionally anchored with [3-(methacryloyloxy)propyl]trimethoxysilane. After the evaluation of physico-chemical parameters of the composite material, it was found that the imprinting effect is strongly dependent on pH of the system environment. The enhanced enantioselectivity of the S-propranolol imprinted copolymer membrane at a higher pH equal to 7.4 has to be related to increased binding of the favored S-enantiomer in the cavity of the polymer. The in vitropercutaneous permeation studies of R/S-propranolol were performed. The results revealed that the S-propranolol imprinted polymer composite of cellulose membrane showed an enantioselectively controlled release of the eutomer of the drug, but the enantioselectivity decreased with an increased concentration during the loading procedure. In a further study [48], the optimized composite of S-propranolol imprinted polymer and cellulose membrane was a part of transdermal patches in order to provide in vivopharmacokinetics. For comparison, the gels containing the racemic drug formulation were also evaluated. The calculated values of AUC were as follows: 715 (for R) and 3928 (for S) for the imprinted patches and 2568 (for R) and 2394 (for S) ng h− 1 mL− 1 for the gels. The significant difference in the concentration of the eutomer after administration of the imprinted transdermal patch confirmed the utility of the novel device. However, the homogeneity of the membrane was unsatisfactory. Thus, S-propranolol imprinted polymer nanoparticles on microspheres were obtained for such a purpose. This material was characterized by the in vitro study, showing its ability to make a controlled release of S-propranolol [49].
Apart of the molecularly imprinted transdermal patches that were extensively studied in the literature, the imprinted subcutaneous implant systems could be different drug delivery forms for dermal administration that could offer delivery of the drug in programmable manner [50].
4.3. Imprinted nanoparticles for intravenous route of administration
The elicitation of all benefits of molecular imprinting technology as well as the investigations of new areas for drug delivery application imposes the quest for new formats of polymers and shifts the material seizure to nanoscale. The imprinted drug delivery nanodevices can be a versatile tool in modern anticancer therapy. Here, intensive studies were performed using 5-fluorouracil as the model drug. This anticancer agent is widely used in clinical treatment, but it is quickly metabolized in the body. An insufficient level of the drug in serum decreased the therapeutic activity and prolonged the treatment. On the other hand, continuous drug administration provoked severe toxic effects [51]. Thus, in order to improve its therapeutic performance and reduce toxic side effects, new drug delivery forms for 5-fluorouracil are still under investigation.
In early works, 5-fluorouracil imprinted submicroparticles were fabricated from methacrylic acid and ethylene glycol dimethacrylate [52]. The adsorption and in vitro release experiments revealed that the imprinted polymer binds 5-fluorouracil much more strongly than the non-imprinted one, and shows a sustained release for a period of 30 h. However, the above material had the following limitations: submicroscale particles are not appropriate for intravenous administration, the precise targeting of cancer cells is impossible, and the polymer matrix is not biodegradable. Thus, to overcome the above problems, new magnetic nanoparticles were fabricated for control delivery of 5-fluorouracil [20]. In the construction process, the Fe3O4 core of nanoparticles was coated with a thin layer of polydopamine imprinted by the 5-fluorouracil template. The core allows one to provide magnetic properties to the nanoparticle which can be used to guide the nanodevice to a disease site by applying an external magnetic field. Such a property of the imprinted nanocarrier is very promising in targeted delivery of a drug. Moreover, the size of particles was appropriate for intravenous administration with an average diameter between 58 and 171 nm. Another advantage is that the polydopamine layer can be easily modified and functionalized for different therapies. In the in vivo experiments the mouse breast cancer model was applied with murine mammary adenocarcinoma cells that were transplanted into the flank region of female Balb/C mice. Five test groups were investigated, viz. control without treatment, sham with implanted magnet without treatment, a group treated with only 5-fluorouracil, a group treated with the imprinted nanodevice soaked with 5-fluorouracil without external magnet use, and a group treated with the imprinted nanodevice soaked with 5-fluorouracil with external magnet use. The histopathological analyses revealed that the total score of malignancy in the last group was reduced. It was concluded that the new imprinted nanodevice increased the local release of 5-fluorouracil, enhanced the control of tumor growth and extended the life span of the examined mice. However, during in vitro release experiments a major burst effect was observed, which was a serious drawback. This phenomenon can be explained by non-specific adsorption during loading of a drug and could be related to the heterogeneous population of binding sites. A simple and excellent method to overcome this problem is to produce a restricted access material combined with the imprinted layer [53]. Such material was produced from glycidyl methacrylate as a pro-hydrophilic monomer carrying an epoxide ring and was treated in the acidified medium after polymerization in order to hydrolyze the epoxide ring. The restricted access imprinted material showed a drastically lower hydrophobic non-specific adsorption of the polymer. Moreover, to improve biocompatibility of the imprinted nanocarriers for targeted delivery of 5-fluorouracil the synthetic reagents were modified. Here, a new cross-linker, tannic acid was applied to provide the biodegradable matrix of magnetic nanoparticles [24]. Additionally, fluorescein isothiocyanate was incorporated into the structure of nanoparticles to facilitate their location and distribution control inside the body. A comprehensive physico-chemical analysis of the new material was carried out together with in vitro degradation tests, in vitro cytotoxicity and in vivo release experiments. The degradation studies which are very important considering biomedical application were performed at various pH 3, 7.4 and 11 (for intravenous administration, pH 7.4 corresponds to pH of blood and pH 11 – to more basic kidney environment). The results revealed faster degradation at pH 3 or pH 11 than at pH 7.4. The results confirmed the utility of the novel biodegradable material which after intravenous administration can survive in the physiological blood environment and deliver the drug to the target site followed by removal to kidneys where it could be degraded. The cytotoxicity tests of the imprinted material (without the drug) were performed on NIH/3T3 cell lines and the cell viability did not show any significant difference for 7 days. The biocompatibility was also evaluated on human embryonic kidney (HEK293) cell line ensuring no changes in morphology or cell death symptoms over a period of 3 days. This means that the above material is not toxic for living cells. In vivo experiments were performed on healthy rats to which a certain amount of imprinted drug-loaded nanodevices was injected intravenously. After applying an external magnet into the region of the kidney, fluorescent images were performed after 48 h revealing a high concentration of nanoparticles in this organ. A similar approach was proposed in another paper [23]. Here, the methacryloyl derivative of fructose was applied as a new, biocompatible cross-linker and olanzapine, the second generation of antipsychotic drug, was used as the template. The applied strategy involved fabrication of magnetic fluorescent multi core shell structure of MIP which facilitates the aggregation of the carrier near the target tissue under external magnetic field. The schematic illustration of the preparation procedure of biodegradable magnetic MIP for targeting drug delivery of olanzapine is presented in Fig. 2. The morphological characterization was carried out. The surface morphology and crystalline size growth of composite nanoparticles were studied by transmission electron microscope revealing spherical entities with average diameter of 20 nm (Fig. 3a–c). The narrow size distribution of particles could be related to the effect of solvent used in the fabrication step. The polydispersity index and z-average for MIPs were as follows 0.14 and 58 nm, respectively (Fig. 3d,e). The atomic force microscopy was also employed in the morphological analysis (Fig. 3f,g). The cytotoxicity of MIPs nanoparticles was measured on NIH/3T3 cell-line using MTT viability assay. The results showed no dramatic change in cell viability during 5 days of incubation proving non-toxic nature of MIPs. The fluorescent images of rat to follow targeting olanzapine delivery are presented in Fig. 4a–e. The pharmacokinetics profiles of control and test groups are presented in Fig. 4f.

Fig. 2. A schematic illustration of the preparation procedure of biodegradable magnetic fluorescent molecularly imprinted polymer for targeting drug delivery of olanzapine under external magnet field (OZ – olanzapine, TEOS – tetraethoxysilane, MPS – [3-(methacryloyloxy)propyl]trimethoxysilane, APS – (3-aminopropyl)trimethoxysilane, FITC – fluorescein thiocyanate).
Reproduced with permission from [23].
Fig. 3. Transmission electron microscope image of nanoparticles: (a) Fe3O4(scale bar = 60 nm), (b) Fe3O4@SiO2 (scale bar = 20 nm), (c) Fe3O4@SiO2@MIPs (scale bar = 20 nm), (d) the statistical graph of size distribution with standard deviation, (e) dynamic light scattering of MIPs dispersed in acetonitrile, (f) atomic force microscope image and (g) cross-section profile of the surface of MIPs nanoparticles.
Reproduced with permission from [23].