1. Introduction
Hospitals played critical role in the maintenance of the health status of a country citizen. On the other hand, hospital activities are often accompanied with the generation of diverse inorganic, organic and microbial components usually released without prior treatment into the environment. Hospital waste management has been a major source of concern to the environmental chemist due to the presence of toxic contaminants that exerts harmful impacts on human and aquatic species. According to Ogwugwa et al. [1], daily wastewater generated in the hospital per bed varies from 40 to 120 L in developed countries and 2–50 L in developing countries like Nigeria [2]. Existing general services namely laundry, kitchen, number and type of wards and units, temperature control systems; numbers of outpatient and inpatients; facility age, number of beds, and maintenance procedures; institutional management practices, geographic location, period of services, and season all have impacts on the volume of wastewater generated in any hospital [3]. The water consumption in hospitals has been estimated between 200 and 1200 L per bed per day, with highest values obtained from developed nations and the lowest from developing countries (200–400 L/bed/day) [4]. In industrialized countries, total hospital wastewater output range from 250 to 570 m3 per day, with a fraction of hospital wastewater ranging from 0.2 to 65% flown and processed in municipal wastewater treatment facilities [4].
Hospital wastewater is loaded with several emerging micro-pollutants such as; original or metabolized pharmaceuticals compounds such as anti-inflammatory, anti-diabetic, antiepileptic, pesticides residue, industrial chemicals, perfluorinated compounds, surfactants, personal care products, analgesics, disrupting compounds, endocrine, antibiotics and hormones radioactive elements, and microorganisms such as; fecal coliform, total coliform, pathogens (E. coli, Vibrion Staphylococcus aureus, Salmonella, and Pseudomonas aeruginosa), radio-elements, and heavy metals [5]. Some of these pollutants are categorized as micro-pollutants (10−6 –10−3 mgL−1) or macro-pollutants (>10−3 mgL−1) based on their measured quantities, and the majority have no regulatory status in the environment [6].
Of particular interest are the emerging micro-pollutants, these are natural or synthetic substances not routinely monitored in the environment but have the potential to infiltrate and exert different health problems [7]. These chemicals enters the ecosystem through different point and non-point sources such as release of untreated wastewater generated, half used and expired products, manufacturing processes and excretion of partially mineralized drugs from the body into sewer system [8]. Drugs with active ingredients are metabolized after administration and the unmetabolized active substances are excreted either unaltered compounds, or conjugated with an deactivating agent or a combination of metabolites linked to the molecule [9], For instance, urine accounts for 55–80% of the total unmetabolized active ingredients [10] and partially in faeces, and thus enter the water cycle. Waste generated from laboratory, diagnostic unit, and operating theater through patients make hospitals key providers of these wide range of micro-pollutants [3]. Chemicals, disinfectants, heavy metals, and sterilizants, iodinated contrast media, and radioactive markers are among the active principles of medications and their metabolites [3].
Hospital effluents have a toxicity that is 5–15 times that of an urban effluent and this constitute serious human and environmental risks following organisms exposure to hazardous substances, or infiltration into groundwater [11,12]. Hospitals, on the other hand, are not the only source of pharmaceutical residues found in all wastewater treatment plants due to their micro properties [6]. Regardless of their variations, in most cases, hospital effluents are categorized as having the same pollution load as sewer wastewaters and are released into public sewage systems, and received as an urban wastewater in treatment facility, and treated in the same manner. The predicted concentrations or observed values of pharmaceutical residues in hospital wastewater are calculated using characteristics such active component intake, water consumption per bed, and percentage excretion [9]. Exposure to these pharmaceutically active residual compounds has contributed to the increasing antibiotic resistance, as most bacteria and fungi have ability to destroy the drugs. For instance in United States of America (USA) alone, approximately 2.8 million antibiotic-resistant infections and 35,000 deaths have been reported yearly, thus considered as emerging areas of concern.
Most municipal wastewater treatment plants are designed for the removal of biodegradable compounds such as, carbon, phosphorus, and nitrogen molecules, as well as microorganisms, but not micro-pollutants such as chemical and pharmaceutical residues, and endocrine disrupting compounds [9]. However, Chlorination is sometimes required for the treatment of the total hospital wastewater, and other times the treatment is just required for the effluent from infectious disease units before being discharged into the municipal sewer [13].
Many authors believe that treating urban and hospital wastewaters in a municipal effluent treatment plant is ineffective because it relies on dilution of diverse outputs and did not allow for pollutant isolation [14,15], particularly emerging micro-pollutants and dangerous compounds, from the liquid phase [16]. Micro-pollutants, particularly pharmaceuticals, are difficult to remove from wastewaters because their concentrations are in the range of 10−3–10−6 mg/L, which is significantly lower than that of traditional macro pollutants (COD, BOD5, phosphorus and nitrogen compounds) [17]. Furthermore, emerging micro-pollutants encompass a wide range of compounds with significant variances in their primary features, which influence their behavior and fate in the wastewater treatment process. The biodegradability and physicochemical qualities such as; water solubility, adsorption, and volatilization of typical pollutants found in hospital wastewater determine their removal effectiveness [18]. The features of wastewater treatment plants (that is, tertiary, secondary and primary treatments), operating circumstances (sludge retention time, temperature, pH and hydraulic), reactor type, and other variables are affected by biodegradability and physicochemical qualities [6]. Since there are new analytical standards which are commercially available; the number of emerging micro-pollutants based on recent investigations continue to increase, and more than 300 pharmaceutical residues and conjugates chemical have been identified. Current researches have been to conduct health risk assessment of number of compounds, because of growing evidence of possible influence on aquatic creatures (such as organ abnormalities, genetic lesions, reproductive abnormalities, and behavioral alterations) and antibiotic-resistant genes and bacteria [19], thus, these pollutants are of special concern.
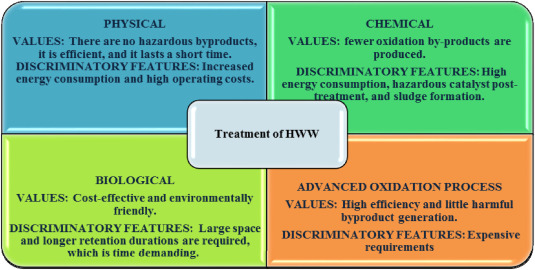
Owing to various problems of hospital wastewater and its derivative, several conventional methods such as; chlorination [20], ozonation [21], reverse osmosis [22], activated carbon adsorption [23], ultra-filtration [24], electro-coagulation [8] have been applied for their removal from wastewater. However, each of the methods has different associated setbacks. For instance, chlorination technology often lead to formation of disinfection by-products (DBPs) which are very more harmful and carcinogenic to human being [25]. Ozonation, and reverse osmosis are very costly [26]. Adsorption technology always generates toxic sludge which occupies space during processing [27]. All these setbacks make it difficult to achieve the desired treatment of wastewater.
On the contrary, advanced oxidation processes (AOPs) have been found suitable for successful removal and degradation of toxicants/pollutants through generation of oxidizing agent (hydroxyl radicals or other free reactive species) [28]. Different researchers have studied degradation of hospital wastewater and its derivatives (such as tetracycline antibiotic, Phenol Forrnaldehyde, Choramphenicol, Norfloxacin, Ciprofloxacin, Dichlofenac, Acetaminophen and Atenolol) using photocatalytic technology [29], Electro-oxidation [30], Electro-fenton [30], Electrocatalysis [31], Ozonation [26], Photo-Fenton [32], Metallic Nanoparticles [33], and Fenton reaction [34]. Most of these techniques are capable of degrading various pollutants nevertheless their efficiency is low [35,36].
Recently, research attention has shifted to hybrid/combination of different treatment techniques to achieve the desired degradation efficiency of emerging micro-pollutants in hospital wastewater within short period of time. In this review paper, the following emerging micropollutants namely Norfloxacin, Ofloxacin, Ciprofloxacin, Clofibric acid, Carbamazepine were selected due to their increase prevalence in the water bodies across the world coupled with the growing cases of bacterial infections rate among patients. Norfloxacin, Ofloxacin and Ciprofloxacin all belong to quinolone antibiotics family used for the treatment of bacterial related infections especially such as urinary tract infections (UTI). Specifically, Norfloxacin is applied primarily to subdue spontaneous bacterial peritonitis (SBP) in patients with liver cirrhosis while Ciprofloxacin is also known for curing SBP in patients. Studies have shown that UTI is one of the most globally prevalence health problem especially among women and out of 8 million patients in one each year, 10 in 25 women and 3 in 25 men usually have symptoms of a UTI. Clofibric acid is an antilipemic agent used for the treatment of hypertrigly ceridemia and high cholesterol. Carbamazepine is a drug used for the treatment of patients’ diagnosed with epilepsy and severe diabetes (peripheral neuropathy). It is estimated that 5 million individuals worldwide are diagnosed with epilepsy each year. Epilepsy is estimated to affect 49 persons out of every 100,000 in high-income nations each year. Each year, 139 people in middle and low-income nations are diagnosed with epilepsy.
Thus, to the best of our knowledge, this is the first review on occurrence, environmental fate, quantification of the selected emerging micro-pollutants in hospital wastewater. The review also provides insight on the different analytical methods for the detection and quantification of the emerging micro-pollutants. The review also provides an overview of the conventional methods of treating hospital wastewater namely: the physical, biological and chemical counterpart. In addition, the review also focus on the theory, mechanism and application of advanced oxidation processes such as photocatalysis, photo-Fenton and combined advanced treatment techniques for the removal of the selected micro-pollutants in hospital wastewater. This state-of-art review also outline new insights on the mechanisms and degradation of the selected emerging micropollutants and formation of various intermediates based on the adopted treatment method.
2. Formation and composition of hospital wastewater
Hospital wastewater encompasses varieties of conventional and non-conventional parameters based on the geographical locations. The formation and compositions (Bacteriological, heavy metals and Pharmaceutical residues) are discussed in this section.
2.1. Bacteriological composition
The evaluation of markers of fecal contamination and pathogens is usually included in the bacteriological composition of hospital wastewater. E. coli is generally used to identify fecal coliforms since it accounts for 80–90% of thermo-tolerant coliforms identified [37]. E coli is a kind of facultative anaerobic bacterium found in the stomach and feaces. The presence of E coli in hospital wastewater indicates fecal pollution, and besides E coli, other harmful fecal microorganisms such as spores of sulfite-reducing anaerobes, Staphylococcus aureus, Salmonella typhii, Pseudomonas aeruginosa; and pathogenic viruses (rotavirus, norovirus, enterovirus, adenovirus) and hepatitis A virus are also exist in high proportion in hospital wastewater [1]. Thus, Enterovirus concentrations have been shown to be 2–3 times higher in hospital wastewater than in municipal wastewater [38].
2.2. Heavy metal composition
Different heavy metals have been found in hospital wastewater [39], such as platinum via excretion by Oncology patients who have been given cis-platinum, carboplatinum, or other cytostatic drugs. [40]; Mercury is widely found in disinfectants, diagnostic agents, and diuretics as active components [5]; and due to gadolinium large magnetic moment, it is often found in iodinated contrast medium used in magnetic resonance imaging [41]. Mercury, and platinum are the most common heavy metals detected in hospital effluents [39]. Other heavy metals, such as copper, lead, cadmium, iron, and nickel, are commonly found in municipal wastewater at similar amounts [39,[42], [43], [44]]. Due to the high magnetic moment imaging of the digestive system, with three magnetic resonance imaging systems serve 15 to 25 patients on a daily basis, spine (MRI), and brain, gadolinium-containing compounds such as gadopentetic acid, gadodiamide, and Gd-diethylenetriamine pentaacetate are delivered (intravenously or orally) regularly. After a few hours of administration, the contrast media are excreted unmetabolized into hospital sewage. It was established that approximately 90% of gadolinium is eliminated during the patient's stay in hospital within 24 h [45], while at home, an excretion rate of 85–98% within 70 min may be achieved. For instance, Oliveira et al. [46], detected gadolinium in effluent from Freiburg University Hospital Germany. Mercury is commonly found in agents of diagnostic, disinfecting active components, and agents of diuretic. In hospital wastewater, mercury contents vary from 0.3 to 7.5 g/L [47]. Since the early 2000s, developed nations have made an attempt to decrease mercury pollution by adopting diagnostic agents without this heavy metal and establishing improved waste management techniques.
Since the mid-1970s, platinum-containing compounds such as; carboplatin and cisplatin, have been utilized as anti-neoplastics in oncology [46]. These antineoplastics are eliminated at various rates after administration (patient dependent). Within the first 24 h following administration, Carboplatin is excreted in 50–75% rate [46]. Cisplatin is excreted between 31 and 85% rate within 51 days after treatment. The two long-term stages of platinum renal excretion have biological half-lives of 160 and 720 days, respectively. 70% of the platinum given is anticipated to be excreted in hospital wastewater [46]. The platinum content was measured by Kümmerer et al. [48], in five European hospitals of various sizes and found to vary between 174 and 2514 beds with concentrations ranging between 3.5 and 0.01 g/L. The authors examined the fluctuation in platinum concentration in the Freiburg University Hospital, Germany over the period of 24 – hour and discovered two concentration maxima at 10 a.m. and 4 a.m. Platinum temporal variability was measured for one week at the main building of the Geneva University Hospital (741 beds – Switzerland) by Daouk et al. [49], who found a significant rise at the end of the week. Platinum concentrations were measured between 0.01 and 2 gL-1 and a ranged of 2.0–289 g/L was found in an oncological unit in Vienna, Austria [50]. They carried out a platinum speciation study and discovered that carboplatin was the major cause of Platinum loading.
2.3. Pharmaceutical residues composition
The use of medicines varies greatly amongst healthcare institutions [51]. For instance, the entire pharmaceutical consumption of a nursing home, a mental hospital, and a regular hospital in Germany has been calculated and varied from 32 kg/year (hospital of psychiatric) to 1263 kg per year (general hospital), with yearly average pharmaceutical consumption ranges between 0.1 and 1000 g per bed [5]. Contrast media, analgesics, antibiotics, laxatives, anti-inflammatories, and cytostatic medicines are the most commonly used therapeutic categories in hospitals [52].
Pharmaceutical residues in hospital wastewater are determined by a combination of three primary factors: the amount given, the fraction excreted, and the chemical properties (primarily biodegradability and stability) [53]. In diverse geographic locations, hospital wastewater have been tested for pharmaceutical residues (Asia – [54], Europe – [55], and North America – [56].
Mayoudom et al. [56], reported the analysis of 12 pharmaceuticals in hospital wastewater and found to have the concentration in range of 78 μgL−1 and 5 mgL−1. The percentage distribution of therapeutic categories is dependent on the analyte under investigation, which usually account for 94% of the total concentrations tested. The most common treatment groups are contrast media, analgesics, cytostatics, and anti-infective and anti-bacterials, which account for more than 40% of the total concentration observed in hospital wastewater [3]. Other identified classes of pharmaceuticals detected include anti-epileptic, psychoanaleptic, anti-inflammatory, and -blocker medications with a maximum concentration of 20% of the total concentration tested [3].
The majority of pharmaceuticals found in hospital wastewater had maximum values of less than 10 g/L [57]. Higher concentrations are usually detected for particular chemicals (such as; ibuprofen, acetaminophen, ciprofloxacin, caffeine, iomeprol, gabapentin, iopamidol, iopromide, theobromine, metformin), with numerous contrast media agents at the low concentration in mgL−1 range [9]. Daouk et al. [49], examined different categories of pharmaceuticals in Geneva University Hospital Switzerland with beds of 741 capacities and calculated mean daily loads to be between 0.1 and 14 g/day for 15 pharmaceuticals, except for piperacillin (0.08 g per day), acetaminophen (143 g per day) and diclofenac (0.04 g per day). The weekly variability of these medicines was explored, and daily load for compounds like morphine, ibuprofen, and acetaminophen, which are often taken on a regular basis, stayed between 50 and 150% of the average [58]. Pharmaceuticals less often used, are mefenamic acid, diclofenac, and the anti-epileptics gabapentin, however have a larger variability, up to 400% of the average value, with the greatest concentrations recorded during the week. Among the medicines studied metronidazole showed more variability than sulfamethoxazole and ciprofloxacin with the greatest amounts of metronidazole detected early in the week.
Compared to general hospitals, specialized wards and hospitals such as; oncologic unit, critical unit, geriatric unit, and psychiatric unit employ a diverse set of medicines. Anti-metabolites and anthracyclines were found in the wastewater of an oncological in-patient care unit (18 beds) at Vienna University Hospital, Austria [50]. In the treatment of lung, bladder, breast, and cutaneous cancer, the anti-metabolite 5-fluorouracil is given in doses ranges between 200 and 1000 mg/m2 body surface [59]. Within 24 h, around 2–35% of the given medication was found unmetabolized in the patient urine [59]. Epirubicin, doxorubicin, daunorubicin, and anthracyclines, are commonly used to treat solid and hematological tumors, such as high-grade lymphoma, acute leukemia, bladder cancer and breast cancer, at doses ranges between 15 and 120 mg/m2body surface [60]. Within 24 h, approximately 3.5–5.7% of doxorubicin, 13–15% of daunorubicin and 11% of epirubicin were found unmetabolized in the urine [61]. 5-Fluorouracil and doxorubicin, which were given as cytostatics, were detected in the wastewater between 8.6 and 124 μg per Lit and 0.26 and 1.35 μg per Lit respectively [62]. The wastewater of the oncological in-patient treatment ward contained 0.5 to 4.5% of the administered quantity of 5-fluorouracil and 0.1 to 0.2% of the administered amount of doxorubicin [63].
de Souza et al. [64], examined intravenous antibiotics used in a Brazilian hospital's intensive care unit (16 beds) and equally estimated the environmental risk and projected environmental concentration (PEC). The usage of antibiotics in the critical care ward is significant because, this unit consumed 25% of all antibiotics even though the unit occupies only 10% of the hospital's entire number of beds are available. Several intravenous antibiotic classes were utilized, with piperacillin, ceftriaxone, ampicillin, meropenem, ceftazidime, cefazolin, sulbactam, clindamycin, trimethoprim, cefepime, and vancomycin having the greatest usage [65]. These researchers computed PECs by taking into account effluent dilution due to surface water flow (10 times) [5]. The estimated concentrations discharged by the critical care unit vary between 1.15 μgL−1 for quinolones to 701 μgL−1 for cephalosporins, if the dilution effect is ignored [66]. Ceftriaxone (320 μg/L) and cefazolin (280 μg/L) have the highest anticipated concentrations among cephalosporins. Penicillins and carbapens are two more groups with substantial anticipated concentrations with 262 μg/L and 229 μg/L respectively. Ampicillin (222 μg/L) and meropenem (220 μg/L) had the highest anticipated concentrations within these two groups [67]. According to de Souza et al. [64], the majority of the intravenous antibiotics studied pose a significant environmental risk. Some of the hazards associated with antibiotic release are due to the emergence of antibiotic-resistant microorganisms [68].
These antibiotics contain adsorbable organic halides, volatile organic and other organic compounds such as phenol, alcohols, acetates, ketones and acetaldehyde [69]. Adsorbable organic halides can be found in pharmaceuticals and disinfectants formed from chlorine applied in cleaning, halogen-containing solvents, and other forms chemical like ethidium bromide [37]. In hospital wastewater, adsorbable organic halides levels range between 150 and 7760 μgL−1, in contrast to the 0.04 to 0.2 μgL−1 range reported in urban wastewaters [37].
2.4. Concentrations of pharmaceutical residues in the hospital wastewater
Predicted and measured concentrations of pharmaceutical residues in hospital wastewater may provide different findings with respect to the time frames used. Projected concentrations are extrapolated from yearly pharmaceutical usage statistics in most circumstances, whereas concentrations are established for a certain time period and at a single point in time [5,70]. Depending on the chemicals, measured concentrations may have more variability than anticipated values. Predicted concentrations are considered by some authors to be a superior choice for determining pharmaceutical discharge over extended time periods [40]. Each technique has advantages and disadvantages that should be considered when building a source characterization attempt. The choice between the two is ultimately determined on access to consumption statistics, cost, and sewage system accessibility, as well as research goals.
Prioritization approaches have been created because the medications are commercially available in hundreds, and many of them can be discovered in the ecosystem as conjugates or parent molecules. These prioritization approaches take into cognizance varieties of parameters such as physico-chemical properties, degradability/persistence, consumption/sales, (eco) toxicity risk, and treatment resistance [6]. Table 1 summarizes various concentration of micro-pollutants (therapeutic drugs) observed in the healthcare facilities effluents. According to this table; there are different classification of pharmaceutical residues such as; Analgesics/inflammatory, antibiotics, anti-hypertensive, psychiatric, beta-blocker, hormones and contrast media. In analgesics, paracetamol was reported to range between 5 and 1,368, ibuprofen between 0.07 and 43, codeine between 0.02 and 50. In antibiotics, ciprofloxacin was reported to range from 0.03 to 125 and norfloxacin between 0.33 and 44.00.
Table 1. Micro-Pollutants: Concentration of Classes of Therapeutic Drugs Measured in Healthcare Facilities wastewater.
| Classification/Analyzed compounds | Concentrations (μg/L) |
|---|---|
| Analgesics/Anti-inflammatories | |
| Paracetamol | 5.00–1368 |
| Ibuprofen | 0.07–43.00 |
| Codeine | 0.02–50.00 |
| Naproxen | 10.00–11.00 |
| Diclofenac | 0.24–15.00 |
| Salicylic acid | 23.00–70.00 |
| Antibiotics | |
| Ciprofloxacin | 0.03–125 |
| Metronidazole | 0.10–90.00 |
| Tetracycline | 0.01–4.00 |
| Ofloxacin | 0.35–35.00 |
| Clarithromycin | 0.20–3.00 |
| Norfloxacin | 0.33–44.00 |
| Penicillin | 0.85–5.00 |
| Doxycycline | 0.10–7.00 |
| Oxytetracycline | 0.01–4.00 |
| Erythromycin | 27.00–83.00 |
| Sulfamethoxazole | 0.04–83.00 |
| Lincomycin | 0.3–2.00 |
| Trimethoprim | 0.01–15.00 |
| Anti-hypertensive | |
| Diltiazem | 0.71–2.00 |
| Psychiatric | |
| Carbamezepine | 0.54–2.00 |
| Beta – blockers | |
| Metoprolol | 0.45–25.00 |
| Hormones | |
| Estrone, E1 | 0.02–0.03 |
| Ethinylestradiol, EE2 | 0.02–0.02 |
| 17β – estradiol, E2 | 0.03–0.04 |
| Estriol, E3 | 0.35–0.50 |
| Contrast media | |
| Iomeprol | 0.01–1392 |
| Iopromide | 0.2–2500 |
| Anti-cancer | |
| 5 – fluorouracil | 5.00–124 |
| Cyclophosphamide | 0.008–2.00 |
| Ifosfamide | 0.01–2.00 |
| Tamoxifen | 0.004–0.17 |
| Anti-diabetics | |
| Glibenclamide | 0.05–0.11 |
| Anti-viral | |
| Aciclovir | 0.02–0.60 |
[3].
3. Adverse effects of hospital wastewater on environment
Pharmaceuticals are excreted as a combination of unmodified parent chemicals and their intermediates (that is metabolite) following ingestion. Although it may appear intuitive that a highly degradable substance (one with a low excretion rate) is easier to break down in the ecosystem, studies have found a negative correlation between the proportion of excreted pharmaceuticals and their concentration in the ecosystem, implying that poorly excreted pharmaceuticals may have a low environmental degradability inherently [71]. Pharmaceuticals may, in fact, take a variety of paths once they enter the sewage system, exhibiting great environmental stability and permanence, or volatilization, and chemical or biological degradation. Drugs such as ciprofloxacin and ceftazidime which contain both basic and acidic functional groups exhibited more complex behavior in sewer network, as well as during wastewater treatment. This means that, depending on the ambient conditions, behavior of these molecules can behave as anionic, cationic, neutral, or zwitterionic in the environment [71]. As a result, understanding the physicochemical features of pharmaceutics can aid in predicting the activities that occur during their passage through wastewater treatment plants. These processes may include biodegradation, or chemical transformation, sorption onto solids, and residual pharmaceuticals may be exposed to photolysis and photodegradation following discharge into surface water bodies, potentially reducing their potential environmental impact [72].
Parent chemicals or modified forms of pharmaceuticals are generally conjugated or hydrolyzed in wastewaters. Hydrolyzed derivatives can lead to the formation of parent compounds at a later period, such as after discharge into a receiving body or during sewage treatment, providing another endogenous source of drug release into the environment [73]. Carbamazepine, for example, is discharged as glucuronides, which may act as a storage for the parent material, which will be released later [74]. To make matters even more complicated, concentrations of some pharmaceuticals have been discovered between the technique's limit of quantification and detection, and consistently below the projected concentration of the environment. This happened, for example, with the anti-neoplastic drug tamoxifen [75], and could be attributed to one or many reasons in this case. One theory is that tamoxifen gets deteriorated before being analyzed because the compound is reported to be UV radiation sensitive, degrading by up to 90% in just 5 days [75]. Photodegradation could not be completely prevented in this case, despite the fact that the analysis was performed as rapidly as feasible and the samples were shielded from light in the meanwhile. Tamoxifen's high lipophilicity (measured log Kow = 6.3) allows it to easily bind to particle detritus that settles to the bottom of sewage systems, avoiding detection [76].
Another explanation for the discrepancy between measured and expected tamoxifen concentrations could be an overestimation of PEC due to the adoption of an improperly inflated unaltered compound excretion rate [77]. After the treated wastewater passed through treatment plants, the remaining active pharmaceutical ingredients may degrade further in surface water bodies. Indeed, if a substance is sensitive to light, photodecomposition may aid the degradation in the environment. Phototransformation is straightforward in clear surface water, and the efficiency of the process is proportional to the frequency and intensity of available light [78]. Other variables, such as water hardness, pH, season, location, and latitude, may, however, influence this process [79]. Despite the fact that tetracyclines, quinolones, and sulphonamides among others are light-sensitive antibiotics, not all antibiotics are photodegradable [80]. Indeed, relevance of each antibiotics and their amount of direct and indirect photolysis in the aquatic ecosystem are different. Therefore, there is need to review the following selected organic pollutant; norfloxacin, ofloxacin, ciprofloxacin, clofibric acid and carbamazepine due to their high rate of consumption which result to their recalcitrant and persistence nature in environment most especially in hospital wastewater.