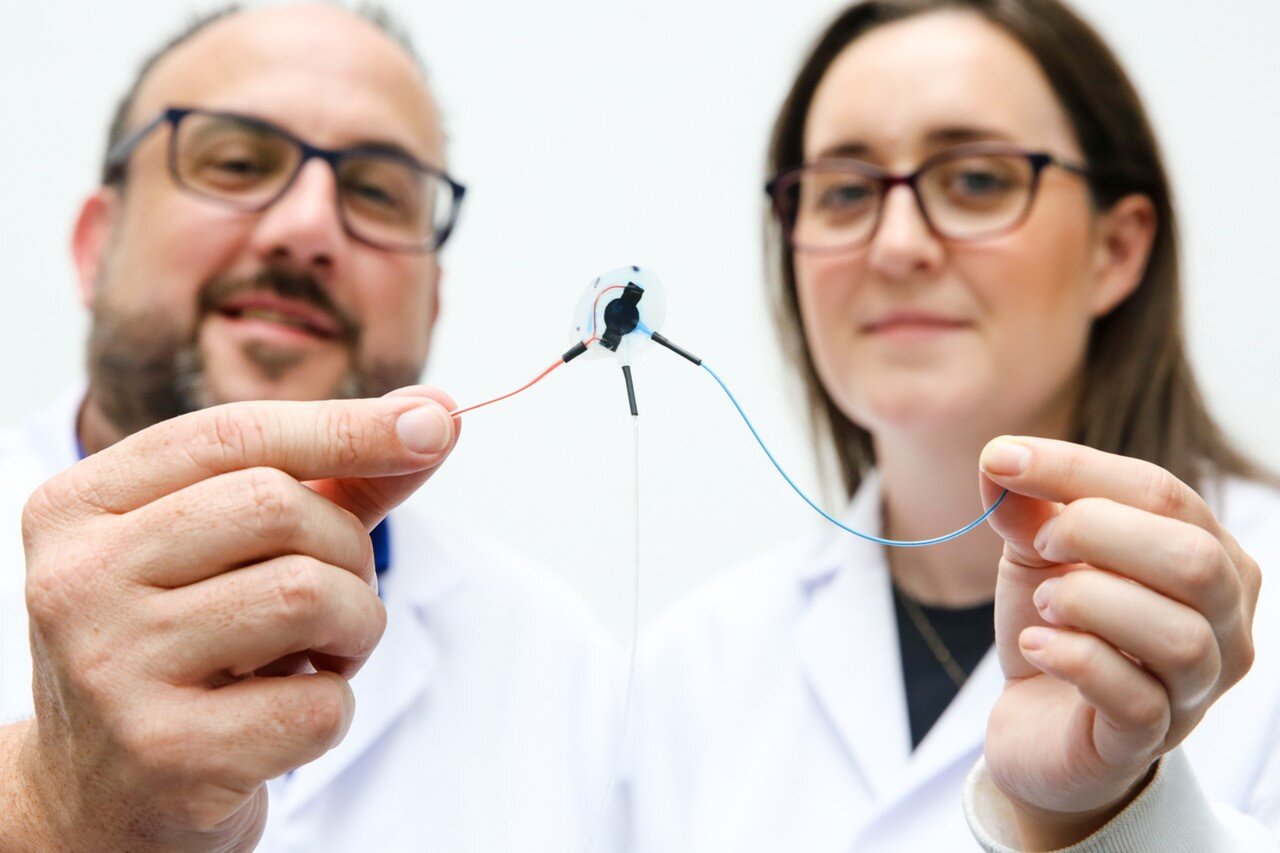
The transatlantic partnership has created a smart implantable device that can administer a drug -- while also sensing when it is beginning to be rejected -- and use AI to change the shape of the device to maintain drug dosage and simultaneously bypass scar tissue build up.
The study was published in the journal Science Robotics.
Implantable medical device technologies offer promise to unlock advanced therapeutic interventions in healthcare, such as insulin release to treat diabetes, but a major issue holding back such devices is the patient's reaction to a foreign body.
Dr Rachel Beatty, University of Galway, and co-lead author on the study, explained: "The technology which we have developed, by using soft robotics, advances the potential of implantable devices to be in a patient's body for extended periods, providing long-lasting therapeutic action. Imagine a therapeutic implant that can also sense its environment and respond as needed using AI -- this approach could generate revolutionary changes in implantable drug delivery for a range of chronic diseases."
The University of Galway-MIT research team originally developed first-generation flexible devices, known as soft robotic implants, to improve drug delivery and reduce fibrosis. Despite that success, the team regard the technology as one-size-fits-all, as it did not account for how individual patients react and respond differently, or for the progressive nature of fibrosis, where scar tissue builds around the device, encapsulating it, impeding and blocking its purpose, eventually forcing it to fail.
The latest research, published today in Science Robotics, demonstrates how they have significantly advanced the technology -- using AI -- making it responsive to the implant environment with the potential to be longer lasting by defending against the body's natural urge to reject a foreign body.
Dr Beatty added: "I wanted to tailor drug delivery to individuals, but needed to create a method of sensing the foreign body response first."
The research team deployed an emerging technique to help reduce scar tissue formation known as mechanotherapy, where soft robotic implants make regular movements in the body, such as inflating and deflating. The timed, repetitive or varied movements help to prevent scar tissue from forming.
The key to the advanced technology in the implantable device is a conductive porous membrane that can sense when pores are blocked by scar tissue. It detects the blockages as cells and the materials the cells produce block electrical signals travelling through the membrane.
The researchers measured electrical impedance and scar tissue formation on the membrane finding a correlation. A machine learning algorithm was also developed and deployed to predict the required number and force of actuations to achieve consistent drug dosing, regardless of the level of fibrosis present. Using computer simulations, the researchers also explored the potential of the device to release medication over time with a surrounding fibrotic capsule of different thicknesses.
The research showed that changing the force and number of times the device was compelled to move or change shape allowed the device to release more drug, helping to bypass scar tissue build-up.
Professor Ellen Roche, Professor of Mechanical Engineering at MIT, said: "If we can sense how the individual's immune system is responding to an implanted therapeutic device and modify the dosing regime accordingly, it could have great potential in personalised, precision drug delivery, reducing off-target effects and ensuring the right amount of drug is delivered at the right time. The work presented here is a step towards that goal."
Professor Garry Duffy, Professor of Anatomy and Regenerative Medicine at University of Galway, and senior author on the study, said: "The device worked out the best regime to release a consistent dose, by itself, even when significant fibrosis was simulated. We showed a worst-case scenario of very thick and dense scar tissue around the device and it overcame this by changing how it pumps to deliver medication. We could finely control the drug release in a computational model and on the bench using soft robotics, regardless of significant fibrosis."
The research team believe that their medical device breakthrough may pave the way for completely independent closed-loop implants that not only reduce fibrotic encapsulation, but sense it over time, and intelligently adjust their drug release activity in response.
Professor Duffy added: "This is a new area of research that can have implications in other places and is not solely limited for the treatment of diabetes. Our discovery could provide consistent and responsive dosing over long periods, without clinician involvement, enhancing efficacy and reducing the need for device replacement because of fibrosis."
The research was funded in part by Science Foundation Ireland's Research Centres for Advanced Materials and BioEngineering Research (AMBER) centre and Medical Devices (CÚRAM), the European Union's Horizon 2020 framework and the Mechanical Engineering Department at MIT.